Evidence of chronic undernutrition in late 19th century German
infants of all social classes
Michael Hermanussen ✉
✉
Aschauhof 3, 24340 Eckernförde – Altenhof, Germany.
Christiane Scheffler
University of Potsdam, Human Biology, 14469 Potsdam, Germany.
DOI: https://doi.org/10.52905/hbph2022.2.42
Abstract
125 years ago, European infants grew differently from modern infants. We show weight
gains of 20 healthy children weighed longitudinally from birth to age 1 year, published by
Camerer in 1882. The data illustrate the historically prevalent concepts
of infant nutrition practiced by German civil servants, lawyers, merchants, university
professors, physicians, foresters and farmers. Breastfeeding by the mother was not truly
appreciated in those days; children were often breastfed by wet nurses or received bottled
milk. Bottle feeding mainly used diluted cow’s milk with some added carbohydrates, without
evidence that appropriate amounts of oil, butter or other fatty components were added.
French children from 1914 showed similar weight gain patterns suggesting similar feeding
practices. The historical data suggest that energy deficient infant formula was fed
regularly in the late 19th and early 20th century Europe, regardless
of wealth and social class. The data question current concerns that temporarily feeding
energy deficient infant formula may warrant serious anxieties regarding long-term
cognitive, social and emotional behavioral development.
Keywords: chronic undernutrition, breastfeeding, historical growth, social class, translation
Conflict of Interest: There are
not conflicts of interest.
Citation: Hermanussen, M. / Scheffler, C. (2022). Evidence of chronic undernutrition in late 19th century German
infants of all social classes. Human Biology and Public Health 2. https://doi.org/10.52905/hbph2022.2.42.
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 27-07-2022 | Accepted: 07-10-2022 | Published: 05-12-2022
Take-home message for students
Historical data suggest that energy deficient infant formula was fed regularly in late
19th and early 20th century Europe, regardless of wealth and
social class. The data question current concerns that temporarily feeding energy deficient
infant formula may warrant serious anxieties regarding long-term cognitive, social and
emotional behavioral development.
Contents
Introduction
In the late 19th century, European infants grew differently from modern infants.
Whereas their intrauterine growth appears to closely match modern references, with birth
weights that only slightly differed from modern birth weights (Boyd, 1980), postnatal increments in length and weight were markedly
less rapid than suggested by modern standards (Hermanussen
et al., 2018; Wilke et al., 2021). James
Tanner was among the first to plot a few historical infant weight data on modern reference
charts (Tanner, 1981), but these first compilations
lack information on variation and, in particular, information on infant nutrition.
The history
In 1882, the well-known German physician Johann Friedrich Wilhelm Camerer (1842–1910), a
pioneer in the field of infant and child nutrition and metabolism, who also contributed
important work on the composition of breast milk, meticulously described feeding and weight
gain in 20 healthy infants and one large for gestational age child (Camerer, 1882). The data, though certainly not obtained from a truly
representative sample, illustrate the historically prevalent concepts of infant nutrition
practiced by German civil servants, lawyers, merchants, university professors, physicians,
foresters and farmers. Quite in contrast to modern practice, breastfeeding by the mother was
not truly appreciated in those days – only child #13, until day 146, and child #15 were fed
in this way. Children were often breastfed by wet nurses (the twin children #3 and #4 until
day 93, the children #5 and #6, child #14 and child #16) or received bottled milk of various
composition. The details of the feeding practices are shown in the appendix 2.
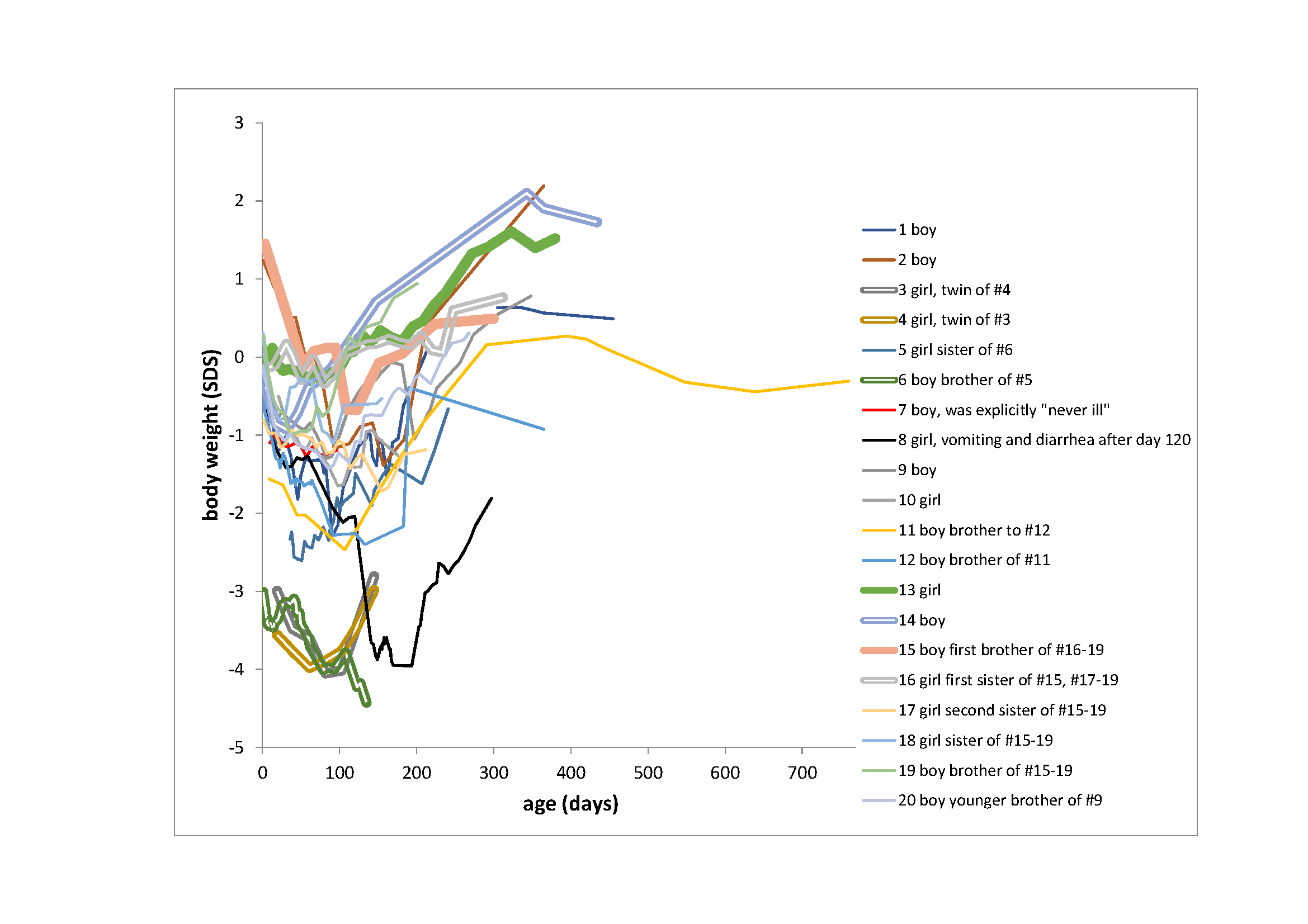
Except for the two breastfed children (#13 and #15), the weight increments of Camerer’s
infants were poor (Figure 1). Particularly wet nurse
feeding appeared unsatisfying, except for child #16, where Camerer explicitly mentioned the
qualification of the nurse, and child #14, the seventh child of a senior staff physician who
presumably was well aware of appropriate child feeding practices. It is worth mentioning
that Camerer did not comment on any of these weight curves, possibly because the incremental
patterns of the majority of his children closely resembled infant weight increments of other
late 19th century authors.
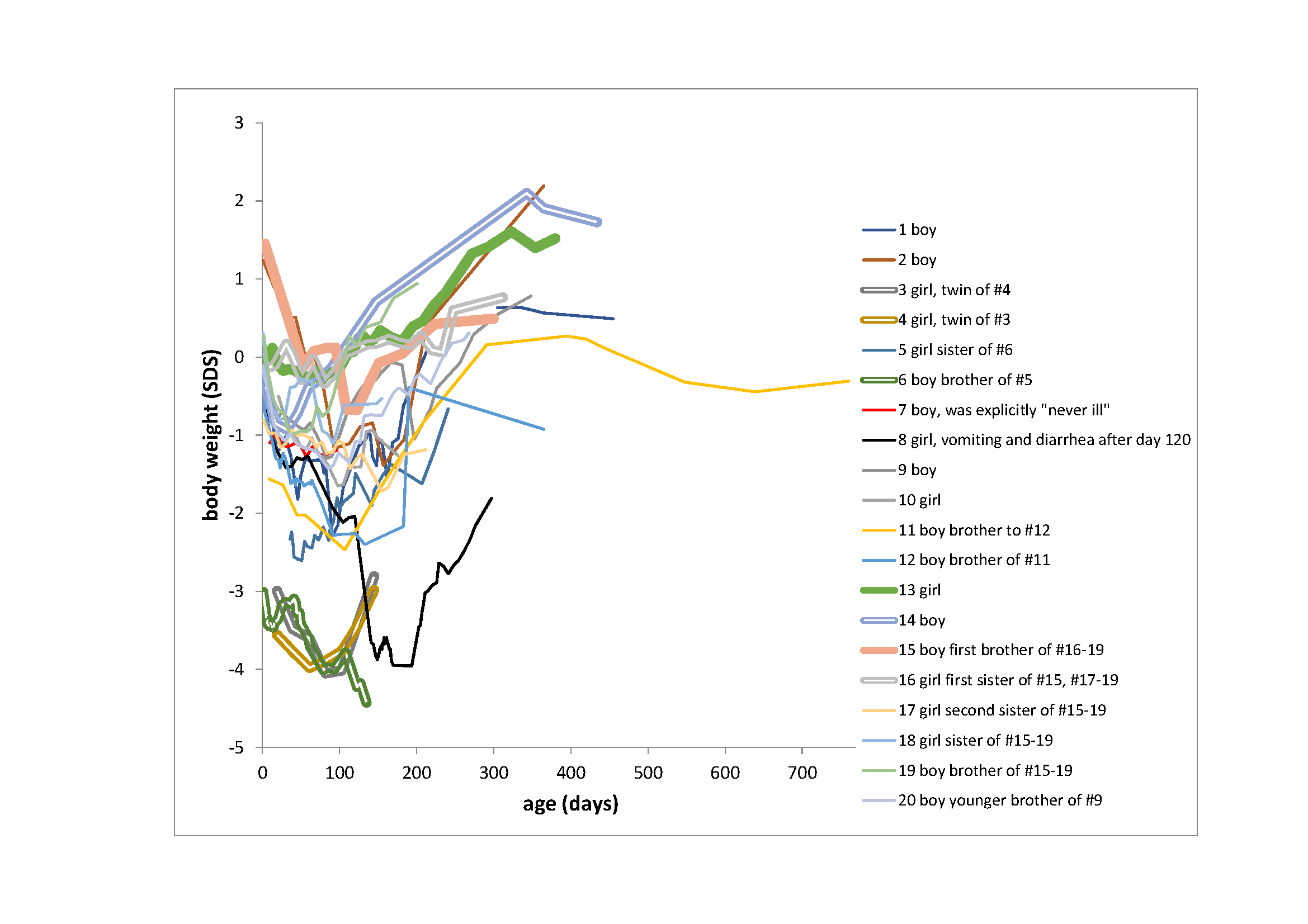
Figure 1
Body weight SDS (WHO, 2006) of 20 infants published
by Camerer in 1882. Thick lines indicate maternal breastfed children, double lines indicate
wet nurse breastfed children, thin lines indicate bottle feeding. The majority of the children
rapidly decline in weight shortly after birth when compared with modern standards.
Camerer also published nutritional details of the bottle feeding. Table 1 (appendix) compiles
estimates of the daily caloric intake of child #19, which were especially well documented.
Feeding mainly used diluted cow’s milk with some added carbohydrates. In this context it is
surprising to note that the documents lack any comment on adding oil, butter or other fatty
components, suggesting that the usual formulas for preparing infant milk propagated in those
days were badly energy deficient (Droese and Stolley,
1961). Interestingly, French children presented in 1914 by Variot (Variot, 1914) showed
very similar weight gain patterns, suggesting similar feeding practices.
Conclusion
Camerer’s article is of particular interest when considering the modern perception of a
pivotal role of nutrition for optimum brain development (Cusick and Georgieff, 2016). Our interpretation of Camerer’s article strongly
questions the 21st century conviction that temporarily feeding energy deficient
infant formula during the first 1000 days of life warrants serious anxieties regarding
long-term cognitive, social, and emotional behavioral development. It seems that energy
deficient infant formula was fed regularly in late 19th and early 20th
century Europe and that many future lawyers, doctors, and professors received insufficient
caloric intake during the first 1000 days of their lives (Matonti et al., 2020).
Generalizing statements such as “Childhood malnutrition is associated with impaired
neurodevelopment, academic achievement, cognition and behavioral problems” (Kirolos et al., 2022) and “Macronutrient (protein, fat,
glucose) sufficiency is essential for normal brain development. Early macronutrient
undernutrition is associated with lower IQ scores, reduced school success, and more
behavioral dysregulation” (Schwarzenberg et al.,
2018), thus, appear inappropriate and may prompt false decisions in public health
and clinical policies. The marked insensitivity of healthy infants to even serious temporary
undernutrition appears to support the idea that the abundant fetal fat deposition during the
last months of pregnancy serves as an efficient energy buffer against nutritional
disruptions that are common at birth and until lactation is established (Kuzawa, 1998; Thayer
et al., 2020).
Appendix
Table 1
Estimated daily caloric intake of child #19. Milk was diluted with water at various
partitions from day 2 to day 34 of life and thereafter was given undiluted. After day
54, milk was diluted with rice mucilage. According to modern references, a healthy
child from 1 month to 1 year of age should receive around 100 kcal/kg/day. Neonatal
(birth to 28 days) caloric requirements are higher at about 110–135 kcal/kg/day (Patel and Rouster,
2022).
|
|
milk |
water/rice mucilage (after day 54) |
|
|
| day |
ml |
partition |
partition |
kcal/day |
kcal/kg/day |
| 2 |
10 |
1 |
2 |
2.3 |
0.7 |
| 3 |
60 |
1 |
2 |
14.0 |
3.9 |
| 4 |
70 |
1 |
2 |
16.3 |
4.6 |
| 5 |
150 |
1 |
2 |
35.0 |
9.9 |
| 6 |
240 |
1 |
2 |
56.0 |
15.8 |
| 7 |
238 |
1 |
2 |
55.5 |
15.6 |
| 8 |
274 |
1 |
2 |
63.9 |
18.3 |
| 9 |
310 |
4 |
5 |
96.4 |
27.6 |
| 10 |
320 |
4 |
5 |
99.6 |
28.5 |
| 11 |
315 |
4 |
5 |
98.0 |
28.0 |
| 12 |
325 |
1 |
1 |
113.8 |
32.5 |
| 13 |
295 |
1 |
1 |
103.3 |
29.5 |
| 14 |
340 |
1 |
1 |
119.0 |
34.0 |
| 15 |
365 |
1 |
1 |
127.8 |
36.0 |
| 16 |
330 |
1 |
1 |
115.5 |
32.6 |
| 17 |
450 |
1 |
1 |
157.5 |
44.4 |
| 18 |
370 |
1 |
1 |
129.5 |
35.3 |
| 19 |
368 |
1 |
1 |
128.8 |
35.1 |
| 20 |
370 |
1 |
1 |
129.5 |
35.3 |
| 21 |
410 |
10 |
9 |
151.1 |
41.2 |
| 22 |
315 |
10 |
9 |
116.1 |
31.6 |
| 23 |
470 |
10 |
9 |
173.2 |
47.2 |
| 24 |
385 |
10 |
9 |
141.8 |
38.7 |
| 25 |
350 |
10 |
9 |
128.9 |
35.2 |
| 26 |
435 |
6 |
5 |
166.1 |
45.3 |
| 27 |
440 |
6 |
5 |
168.0 |
45.8 |
| 28 |
330 |
6 |
5 |
126.0 |
32.7 |
| 29 |
305 |
6 |
5 |
116.5 |
30.2 |
| 30 |
440 |
6 |
5 |
168.0 |
43.6 |
| 31 |
355 |
6 |
5 |
135.5 |
35.2 |
| 32 |
390 |
6 |
5 |
148.9 |
38.6 |
| 33 |
370 |
6 |
5 |
141.3 |
36.6 |
| 34 |
375 |
6 |
5 |
143.2 |
37.1 |
| 35 |
385 |
only cow’s milk |
|
269.5 |
68.8 |
| 36 |
440 |
only cow’s milk |
|
308.0 |
78.7 |
| 37 |
405 |
only cow’s milk |
|
283.5 |
72.4 |
| 38 |
360 |
only cow’s milk |
|
252.0 |
64.4 |
| 39 |
295 |
only cow’s milk |
|
206.5 |
52.7 |
| 40 |
265 |
only cow’s milk |
|
185.5 |
47.4 |
| 41 |
395 |
only cow’s milk |
|
276.5 |
70.6 |
| 42 |
395 |
only cow’s milk |
|
276.5 |
66.9 |
| 43 |
395 |
only cow’s milk |
|
276.5 |
66.9 |
| 44 |
330 |
only cow’s milk |
|
231.0 |
55.9 |
| 45 |
400 |
only cow’s milk |
|
280.0 |
67.7 |
| 46 |
450 |
only cow’s milk |
|
315.0 |
76.2 |
| 47 |
420 |
only cow’s milk |
|
294.0 |
71.1 |
| 48 |
520 |
only cow’s milk |
|
364.0 |
88.0 |
| 49 |
395 |
only cow’s milk |
|
276.5 |
66.9 |
| 50 |
385 |
only cow’s milk |
|
269.5 |
65.2 |
| 51 |
475 |
only cow’s milk |
|
332.5 |
75.6 |
| 52 |
480 |
only cow’s milk |
|
336.0 |
76.4 |
| 53 |
540 |
only cow’s milk |
|
378.0 |
85.9 |
| 54 |
380 |
only cow’s milk |
|
266.0 |
60.5 |
| 55 |
480 |
5 |
7* |
184.8 |
42.0 |
| 56 |
410 |
5 |
7 |
157.9 |
35.9 |
| 57 |
510 |
5 |
7 |
196.4 |
42.6 |
| 58 |
475 |
5 |
7 |
182.9 |
39.7 |
| 59 |
510 |
5 |
7 |
196.4 |
42.6 |
| 60 |
510 |
5 |
7 |
196.4 |
42.6 |
| 61 |
520 |
5 |
7 |
200.2 |
43.5 |
| 62 |
400 |
5 |
7 |
154.0 |
33.4 |
| 63 |
465 |
5 |
7 |
179.0 |
38.9 |
| 64 |
525 |
5 |
7 |
202.1 |
41.6 |
| 66–72 |
470 |
5 |
7 |
181.0 |
37.2 |
| 73–78 |
525 |
5 |
7 |
202.1 |
38.4 |
| 79–80 |
665 |
5 |
7 |
256.0 |
47.4 |
| 81–88 |
570 |
5 |
7 |
219.5 |
38.8 |
| 89–93 |
595 |
5 |
7 |
229.1 |
38.1 |
| 93–106 |
690 |
5 |
7 |
265.7 |
49.9 |
| Thereafter |
805 |
5 |
7 |
309.9 |
47.0 |
Appendix 2: Description of infant growth, a partial translation of Camerer,
1882
1st* Boy, 2nd child, age of parents 39 and 25 years, social status
unknown, residence Würzburg. Food: 1st week breastmilk; 2nd to
4th week breastmilk and Nestle's flour with cow's milk; 4th to
7th week Nestle and cow's milk alone; 7th to 12th week
(because of small weight gain with Nestle) 2 parts cow's milk, 1 part water, some rusk flour;
12th week without proper food because of diarrhea; 13th to
17th week nurse milk and Liebig's soup; 18th to 23rd week
Liebig's soup and milk with rusk meal (temporarily without proper food in the 21st
and 23rd week because of diarrhea). From the 24th week to the
1st year cow's milk and rusk flour (at ½ year, 1½ liters of milk and 4
tablespoons of rusk flour were consumed per day). At the age of 1 year, besides milk and rusk
flour, meat broth soup. Illnesses: severe flu at age 9 month.
2nd* Boy, 4th child, age of parents 40 and 32 years, civil servant,
Stuttgart. Food: cow's milk. Birth weight unknown, estimated by physician at a little over 4
kilos. Illnesses: at the beginning of the 4th month severe eczema, at the beginning
of the 6th month severe recurrence of the previously not completely healed eczema.
3rd* and 4th* are twins, girls, 2nd and 3rd
child, age of parents 43 and 31 years, lawyer, Stuttgart. Food until 93rd day:
nurse milk, from then until 152nd day milk and Nestle’s infant cereal cooked in
meat broth.
5th* and 6th* are siblings. The first child a girl, age of parents 30
and 20 years, civil servant, Karlsruhe, food: cow's milk and gruel; the 2nd child a
boy, age of parents 31 and 21 years, food: nurse milk, nurses were changed twice. The mother
died of puerperal fever on the 34th day after the birth of the 2nd
child.
7th* Boy, 3rd child, age of parents 38 and 37 years, merchant,
Tübingen. Food: for the first 63 days cow's milk and anise tea, then cow's milk and barley
gruel (1 tablespoon of barley with 125 grams of fat-free ox meat and 1 liter of water boiled
down to ½ liter of liquid). The child was never sick.
8th* Girl, 2nd child, age of parents 40 and 26 years, professor,
Tübingen. Food: Cow's milk with chamomile tea. From the 120th day diarrhea and
vomiting for a long time.
9th* Boy, 1st child, age of parents 26 and 20 years, general practitioner in
Königsbronn, Württemberg. Food: In the 1st week breastmilk; in the 2nd
week breastmilk and diluted cow's milk (1 milk, 2 water, some sodium carbonate and lactose).
From the 3rd to the 10th week, diluted cow's milk alone; finally, the
mixture consisted of 4 milk and 3 water, always with sodium carbonate and lactose. The child
drank an average of 120 ml milk and 90 ml water per meal in the 9th week. In the
11th week, an attempt to add some rusk flour to the diluted milk induced
diarrhea, so they returned to the previous diet. In the 13th week, the child drank
220 ml milk and 50 ml water per meal, in the 18th week 270 ml pure milk (with
sodium carbonate and lactose) and 1300 ml per 24 hours. From the 20th week, some
rusk flour was given together with the milk, at this time 260 ml milk were consumed at a
single meal and per day some 1500 ml. The feces were always normal, except in the
11th week; they became harder, so that enemas became necessary when the milk (in
the mixture) was increased. From the 186th to the 193rd day severe
emetic diarrhea (temperature up to 39.9); various feeding attempts failed until at last, with
exclusive use of Nestle's flour boiled with water, the illness ceased without medication. On
the 192nd day 7 tablespoons of flour and 490 ml of water were consumed; thereafter
per 24 hours until the 197th day: 80 g of flour; until the 201st day:
100 g of flour, then 114 g and 145 g, the latter amount was not exceeded. From the
212th day: milk was again added to Nestle's flour, starting with one meal of milk
porridge of 130 grams and soon increasing again to 1200 grams of milk per day. From the
250th day the child was given 1 soft egg in the morning. In the 10th
month the diet was: egg in the morning, soup of meat broth and bread at noon, 1 tablespoon of
Nestle boiled with 260 grams of water, 4 portions of milk of 260 grams during the day. From
the 160th to the 170th day the child suffered from bronchial catarrh; at
14 months he could walk freely.
10th* Girl, 1st child, age of parents 37 and 23 years, professor,
Tübingen. First-born sister of No. 8. Mostly fed on condensed milk.
11th* and 12th* are siblings, both boys. Parents 42 and 30 years old at
1st child's birth, 43 and 31 years old at 2nd child's birth. Head
forester, Riedlingen. Food for both children: diluted cow's milk.
13th* Girl, 1st child, age of parents 36 and 31 years. Head forester,
Steinheim, Württemberg. Food: until 146th day exclusively breastmilk, from then
until 223rd day breastmilk and complementary food (first based on cow's milk, at
the end of the period cow's milk and meat soup). Completely weaned on the 223rd
day. End of 1st year 6 teeth, walking on one hand.
14th* Boy, 7th child. Parents 40 and 39 years old. Senior staff
physician, Ulm. Feeding: 7 months exclusively nurse milk; 7–9 months nurse milk with
additional food, namely a semolina soup with an egg during the day; from 9–11 months a soup of
cow's milk and bread flour in the evening; from 11 months without breastmilk with cow's milk
and soups. At the end of the 11th month with 4 teeth, at the end of the
12th month with 7 teeth; walks led by one hand, is unusually muscular and
lively.
The following 5 children are siblings, the weighing was done by the mother (as with several
of the children mentioned here) and kindly left to me. May these women find many
successors!
15th* Boy, 1st child. Parents 38 and 27 years old, professor, Tübingen.
Feeding during the first 4 months breastmilk and nurse's milk. 4 wet nurses, only the
4th had enough milk and stayed until the 12th month; during the change
of wet nurses Liebig's soup and cow's milk was given. The child never suffered from
indigestion. Around 100 days of life, large boil on thigh.
16th* Girl, 2nd child. Age of parents 40 and 29 years. From the
3rd to the 10th month an excellent wet nurse.
17th* Girl, 3rd child. Age of parents 42 and 31 years. Food: beside and
between 3 insufficient wet nurses cow's milk, from the 4th month only cow's milk.
In the 5th month pneumonia and scarlet fever.
18th* Girl. 4th child, age of parents 45 and 34 years. In the first 6
weeks trials with wet nurses, thereafter until the 7th month fed exclusively with
Nestle. Had 4 teeth in the 7th month, could almost walk alone at 12 months.
19th* Boy, 5th child, age of parents 49 and 38 years. Child got 2 first
teeth on 189th and 197th day of life. Food: diluted cow's milk. From day
1 to 34 of life, milk was diluted with water (first 8 days, 1 milk:2 water; 9th,
10th, and 11th days, 4:5; 12th–20th day1:1;
21st–25th day, 10:9; 26th–34th day, 6:5). From
day 54 to 150, the milk was diluted with rice water and rice mucilage; initially the mixing
ratio was 5 milk:7 mucilage, and finally 2 milk:1 mucilage. From about the 150th
day, veal broth was added to the milk once a day; otherwise, the milk was diluted with water
(5 milk to 1 water) (details: see table 1).
The number of daily meals averaged 6.7 from day 3 to 27; the minimum of 5 and the maximum of
8 meals occurred twice. From day 28 to 68 of life, the number of daily meals averaged 6; the
minimum of 5 occurred 13 times, and the maximum of 7 occurred 9 times. From the
69th to the 120th day the number of daily meals was again 6.5; the
minimum was 6, the maximum 7. At the 1st day none, at the 2nd day one meal with 10
grams of milk is noted.
20th* boy, 2nd child, brother of No. 9. Age of parents 28 and 22 years.
Illnesses: mild measles from the 107th to the 110th day; bronchial
catarrh on the 260th and following days. Food: in the first 13 days sparse
breastmilk; complementary food: milk and water with some sodium carbonate and lactose: mixture
at the beginning 1 milk: 2 water; at the end 3 milk to 4 water. From the 180th day
on, digestive disturbances occurred. Therefore, the previous milk regime was completely
suspended and only Nestles flour boiled with water, was given. The same from the
210th to the 214th day. Thereafter, the flour was gradually
discontinued and cow's milk was added, and on about the 230th day pure cow's milk
was given again. A similar procedure was done on day 270 and the following days. Nestle's
flour was first boiled with water, during the following weeks, cow's milk was given again.
Diarrhea also occurred on the 320th day when pure cow's milk food was given, the
stools were slimy, contained some blood and pus cells. Slight increases in temperature. A
trial with Nestle's meal and Biedert's cream mixture was unsuccessful. Enemas with starch
flour and tannin were then given, and acorn coffee and cream internally; whereupon the disease
subsided. The child soon switched to a mixed diet. The first incisors appeared around the
300th day. At 1 year and 1 month the child could not yet walk, but was close to
it.
21st* boy (not plotted in Figure 1),
7th child, age of parents 49 and 40 years. Farmer, Dürmentingen near Riedlingen.
In this interesting case, unfortunately, only a few and not entirely accurate weighings could
be made (the possible weighing error is up to 250 grams), nevertheless it seems to me worth of
a report. On the occasion of an operation, I was informed by the assisting surgeon that an
unusually heavy child had been born a few days ago. … The boy was weighed 24 hours after birth
and is said to have weighed 7500 grams. …
My examination on the 10th day after birth revealed the following: Date from onset
of menstruation to birth of the child 299 days. Length of the child 54,4 cm. Head
measurements: circumference 38 cm, longitudinal diameter 13 cm, transverse diameter 10.7 cm.
Breast measurements: shoulder width 13.8 cm, breast circumference (at nipple height) 37 cm,
straight breast diameter 11.4 cm. Distance of troch. major. 10.6 cm, weight 4500 g. Bowel
movements regular. He drank on the 11th and on the 12th day of life 650
ml per day on average, half milk, half water.
Acknowledgements
This manuscript is part of a contribution to a celebratory event held in Tartu, Estonia, October 15th 2022,
in honor of Prof. Juhan Aul.
References
Boyd, E. (1980). Origins of the study of human
growth. Portland, University of Oregon Health Sciences Center Foundation.
Camerer, W. (1882). Gewichtszunahme
von 21 Kindern im ersten Lebensjahre. Jahrbuch der Kinderheilkunde Neue Folge 18,
254–264.
Cusick, S. E./Georgieff, M. K.
(2016). The role of nutrition in brain development: The golden opportunity of the “First
1000 Days.” The Journal of Pediatrics 175, 16–21. https://doi.org/10.1016/j.jpeds.2016.05.013.
DEBInet – Deutsches Ernährungsberatungs- & Informationsnetz (2022). Humana Reisschleim
flussig. Available online at https://www.ernaehrung.de/lebensmittel/de/HUMANA727/Humana-Reisschleim-flussig.php
(accessed 7/26/2022).
Droese, W./Stolley, H. (1961). Kuhmilchfett und
pflanzliches Fett in der Ernährung des jungen, gesunden Säuglings [Cow’s milk fat and
vegetable fat in the feeding of young healthy infants]. Deutsche Medizinische
Wochenschrift 86, 855–860. https://doi.org/10.1055/s-0028-1112867.
Hermanussen, M./Bogin, B./Scheffler, C. (2018). Stunting, starvation and refeeding: a review of forgotten 19th
and early 20th century literature. Acta Paediatrica (Oslo, Norway : 1992) 107,
1166–1176. https://doi.org/10.1111/apa.14311.
Kirolos, A./Goyheneix, M./Eliasz, M. K./Chisala, M./Lissauer, S./Gladstone, M./Kerac, M. (2022).
Neurodevelopmental, cognitive, behavioural and mental health impairments following
childhood malnutrition: a systematic review. BMJ Global Health 7 (7), e009330. https://doi.org/10.1136/bmjgh-2022-009330.
Kuzawa, C. W. (1998). Adipose tissue in human
infancy and childhood: an evolutionary perspective. American Journal of Physical
Anthropology 107 (S27), 177–209. https://doi.org/10.1002/(sici)1096-8644(1998)107:27+<177::aid-ajpa7>3.0.co;2-b.
Patel, J. K./Rouster, A. S. (2022).
Infant nutrition requirements and options, in: StatPearls. Available online at https://www.ncbi.nlm.nih.gov/books/NBK560758/
(accessed 11/24/2022).
Schwarzenberg, S. J./Georgieff,
M. K./Committee On Nutrition/Daniels, S./Corkins, M./Golden, N. H./Kim, J. H./Lindsey, C. W./Magge, S. N. (2018). Advocacy for improving nutrition in the first 1000
days to support childhood development and adult health. Pediatrics 141 (2), e20173716. https://doi.org/10.1542/peds.2017-3716.
Tanner, J. M. (1981). A history of
the study of human growth. Cambridge, Cambridge University Press.
Thayer, Z. M./Rutherford, J./Kuzawa, C. W. (2020). The maternal nutritional buffering model: an evolutionary
framework for pregnancy nutritional intervention. Evolution, Medicine, and Public
Health 2020 (1), 14–27. https://doi.org/10.1093/emph/eoz037.
Variot, G. (1914). Tables des Croissances comparées des Nourissons élevés au sein et au biberon durant la pemière Année de la Vie. Paris, A. Davy.
WHO (2006). WHO child growth
standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height
and body mass index-for-age: methods and development. Available online at https://www.who.int/publications/i/item/924154693X(accessed 7/26/2022).
Wilke, L./Boeker, S./Mumm, R./Groth, D. (2021). The social status influences human growth: A summary and analysis of historical data from German school girls in 1914 with comparison to modern references. Human Biology and Public Health 3. https://doi.org/10.52905/hbph2021.3.22.