“Obesity in the City”
Urbanization and rising obesity rates from the viewpoint of human biology and
public health
Sylvia Kirchengast ✉
✉
University of Vienna, Department of Evolutionary Anthropology, Djerassiplatz
1, A-1030 Vienna, Austria
University of Vienna, Department of Evolutionary Anthropology, Djerassiplatz
1, A-1030 Vienna, Austria
DOI: https://doi.org/10.52905/hbph.v2.11
Abstract
In 2007, for the first time worldwide, more people lived in urban conurbations than in
rural settlement structures. This advancing urbanization has dramatically altered the
living situation, the use of space, as well as human behavior along with the health
situation and disease burden. This process began in Europe as early as the 19th
century, while developing and emerging countries in particular are currently experiencing
an increase in urbanization. The burden of disease is clearly altered by living in a
confined space, by environmental pollution in urban areas, the impossibility of producing
food oneself, and being lost in an anonymous crowd. Obesogenic environments represent a
special problem in urban areas. A lack of physical activity, adverse dietary habits, and
stressful and unsafe neighborhoods increase the risk of becoming overweight and obese in
urban centers. Recently, modernization in rural areas and an adaptation to urban habits
there increase the obesity rates in rural areas in high-income as well as low- and
middle-income countries, too. Within cities, marked spatial differences in the prevalence
of overweight and obesity occur. In Vienna, Austria, overweight and obesity rates during
childhood and adolescence differ markedly between the individual Viennese districts.
Highest overweight and obesity rates occur in districts characterized by a low
socio-economic status.
Keywords: childhood obesity, spatial differences, Vienna, gender
Conflict of Interest: There are no
conflicts of interest.
Citation: Kirchengast, S.,Hagmann, D., (2021), “Obesity in the City”, Human Biology and Public Health 2. https://doi.org/10.52905/hbph.v2.11.
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 25-12-2020 | Accepted: 09-04-2021 | Published: 23-12-2021
Take home message for students
We are currently confronted with the greatest wave of urbanization in the history of
Homo sapiens. Urbanization is not only associated with
modernization and cities are not only economic and cultural centers and areas of
inspiration. Urban centers are also associated with increased psychic and somatic stress,
health risks and high rates of obesity.
Contents
Introduction
We are currently living in a rapidly changing world. Climate change, transcontinental
migration, population ageing, over-population, digitalization, globalization and
urbanization represent important stress factors for Homo
sapiens. They have a major impact not only on economic and social development,
but some of those factors also influence biological traits such as growth and development
along with health and disease patterns. This makes the above-mentioned parameters of
particular interest for both human biology and public health studies.
The association between urbanization and obesity prevalence is steadily gaining importance
due to current trends: Twelve years ago, in 2008, a twofold turning point was reached. On
the one hand, in 2007, for the first time, more than 50% of the world's population lived in
urban habitats; the prediction is that this trend will continue in the coming years and
decades (United Nations 2015). On the other hand,
in 2008, for the first time in the long history of Homo
sapiens, the number of overweight and obese people on Earth exceeded the number
of people who suffer from starvation and malnutrition (FAO
2008). The association between both trends, e.g. urbanization and rising obesity
rates is the topic of this review. In detail, urban environments are discussed from the
viewpoint of Evolutionary Anthropology, current urbanization rates and overweight/obesity
rates are presented. Particular attention is paid to obesogenic environments and spatial
differences of obesity rates among children and adolescents in Vienna, Austria.
Obesity – a worldwide public health concern
Without doubt, obesity represents one of the major worldwide public health challenges of
the21st century (Chooi et al. 2019;
Spinelli et al. 2019). Overweight and obesity is
commonly defined as an excessive amount of adipose tissue. Among adults a body mass index
(BMI) above 25.00 kg/m2 is considered overweight, a BMI above 30.00
kg/m2 is considered as obese (WHO
2000). Among children and adolescents. of the same age and sex,
overweight is defined as a BMI at or above the 85th percentile and below the
95th percentile. Obesity is defined as a BMI at or above the 95th percentile
for children and teens of the same age and sex (Aggarwal
and Jain 2018).
Obesity is mainly seen as a very recent phenomenon because at the population level obesity
was rare up to the 1950s (Brown 1991; Haslam 2007). In the second half of the 20th
century, however, obesity rates rose sharply in the high-income countries and later also in
the emerging countries. Once considered a condition typical solely of affluent societies in
the industrialized world, overweight and obesity rates are now fast growing in poor
neighborhoods of high-income countries as well as in many middle- and low-income countries
(WHO 2000; WHO 2010; Hossain et al. 2007; Pijl 2011; Chooi
et al. 2019). Between 1975 and 2016, the world-wide prevalence of obesity nearly
tripled (Blüher 2019). According to the World
Health Organization (WHO), in 2016, more than 1.9 billion adults (≥18 years) were overweight
(BMI > 25.00 kg/m2); of these, 650 million adults were classified as obese.
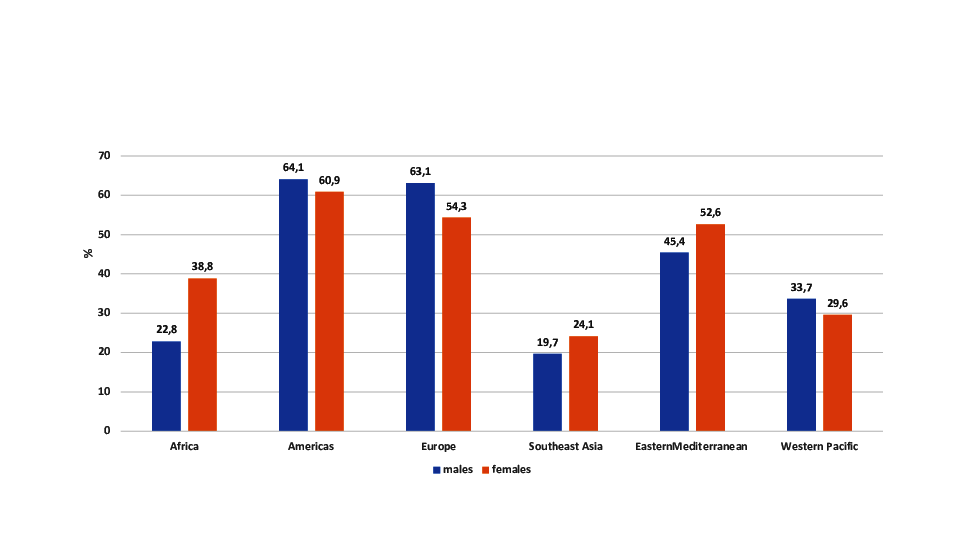
This means that 39% of the world´s adult population were overweight, 13% obese (Chooi et al. 2019; WHO 2020). Figure 1 presents overweight + obesity rates for adult males and
females according to world regions. Lowest overweight and obesity rates are found for
Southeast Asia and Africa. The highest rates are found for the Americas and Europe.
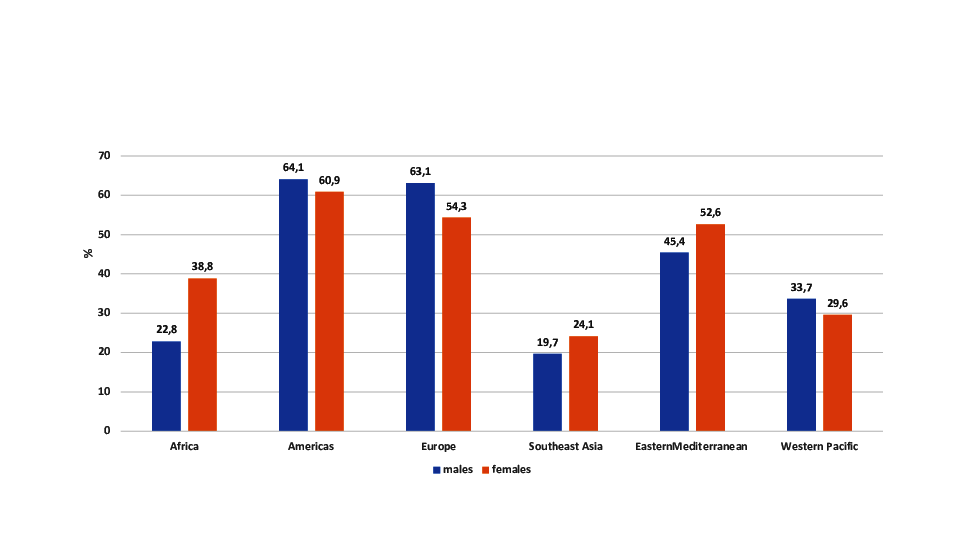
Figure 1 Overweight and obesity rates according to World regions according to the WHO
(WHO 2020).
A special problem is the rising rates of overweight and obesity among children (Spinelli et al. 2019). In 2016, more than 340 million
children and adolescents aged 5-19 years were overweight or obese worldwide. Furthermore,
the prevalence of overweight and obesity among children younger than 5 years has increased
dramatically. In 2019, about 38.2 million children under the age of 5 years were overweight
or obese. This is true not only of high-income countries but also of middle- and low-income
countries (WHO 2020). Currently, nearly half of
the overweight or obese children younger than 5 years live in Asia. In Africa as well,
however, the number of overweight children younger than 5 years has increased by nearly 24%
since 2000.
This high prevalence of excessive body weight worldwide is a matter of concern because
obesity represents an important risk for premature mortality and morbidity (Ford and Mokdad 2008; Wang et al. 2011). Furthermore, overweight and obesity are not merely
individual health problems – they also place an enormous economic burden on public health
and social systems of governments. This makes the analysis of risk factors enhancing the
risk of overweight and obesity ever more important.
From a physiological point of view, overweight and obesity are caused by an imbalance
between energy intake and expenditure (Florentino
2002). On the one hand, this imbalance, is associated with genetic factors. There
is no doubt, that obesity is complex heritable trait (Thaker 2017). Beside monogenic causes such as single gene mutations primarily
located in the leptin- melanocortin pathway, polygenic obesity is caused by a cumulative
contribution of a large number of genes (Thaker
2017). Currently it is assumed that the genetic component may contribute to 40-70%
of obesity (Chiurazzi et al. 2020). On the other
hand, there is a strong environmental component, which may enhance the risk of obesity. The
main environmental reason for rising obesity rates worldwide is the globalization of
increasingly obesogenic environments, which are mainly characterized by rapid urbanization
associated with the mechanization of jobs, improved transportation services, the
availability of food of high energy density, and reduced physical activity (Popkin and Udry 1998; Popkin 2001; Popkin 2003; Popkin and Gordon-Larsen 2004; Poston and Foreyt 1999; Ulijaszek
2007; Ulijaszek and Lofink 2006).
Urbanization – a problem of definition
Urbanization is apparently related to rising obesity rates worldwide. Before we start to
discuss the phenomenon urbanization and its associations with parameters of human biology,
such as growth patterns, but also parameters of public health, in particular obesity rates,
we have to define the terms urbanization, urban environments, urban centers and cities.
Urbanization describes the process by which large numbers of people become permanently
concentrated in relatively small areas, forming urban habitats or cities. To date, no
uniform definition of the terms city or urban centers exists. A city is commonly defined as
a large human settlement, the term "city" however, has different meanings around the world.
Some definitions classify human settlements with more than 250,000 inhabitants as cities,
while and in some places the settlement can be very small indeed. A town in contrast, is
defined as a settlement that is larger than villages, but smaller than cities. An important
trait of cities is, that the inhabitants work primarily on non-agricultural tasks (Caves 2005). Even the United Nations (UN) uses regional
definitions, which vary considerably from state to state. For instance, the United States
defines an urban place as any locality, where more than 2,500 People live. In contrast, in
Peru an urban place is any locality with 100 or more dwellings (Duignan 2019). In Japan, a city is defined as a shi with a minimum of
50,000 inhabitants, while Sweden or Denmark set the threshold at only 200 inhabitants. The
most frequently used thresholds for the definition “urban” are 2,000 to 5,000 inhabitants.
The European Commission defined urban centers as areas with more than 50 000 inhabitants
plus a population density of at least 1500 people per square kilometer (km2).
Urban clusters are defined as areas with a minimum of 5,000 inhabitants plus a population
density of at least 300 people per square kilometer (km2). Every location with
less than 5,000 inhabitants is considered as rural. Therefore, the degree of urbanization
differs depending on the definition. According to the definitions of the European commission
only 15% of the world population lived in rural areas, while 52% lived in urban centers and
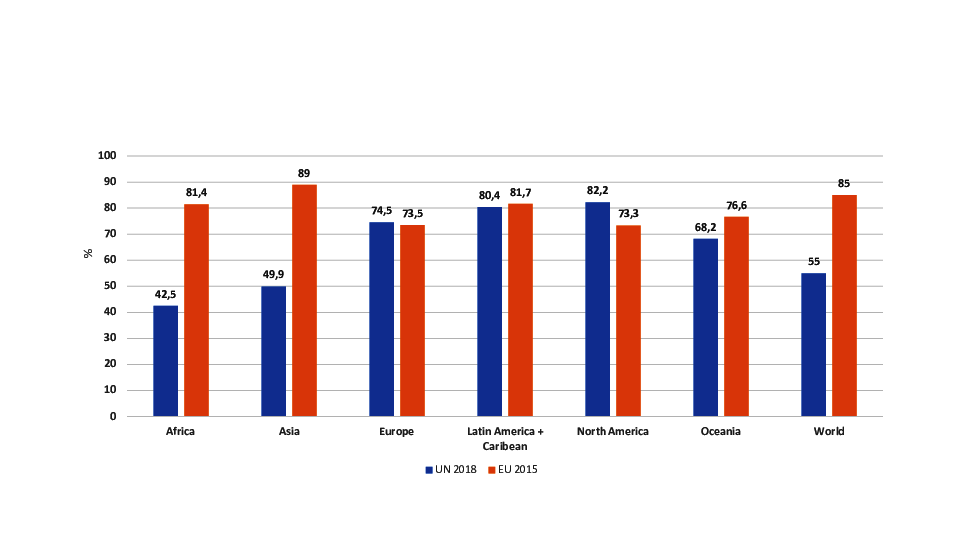
33% in urban clusters in 2016. As presented in Figure 2, major differences in the percentage of urbanization between the UN definition
and the European commission definition occur for Africa and Asia. These differences in the
definitions of urban areas may contribute to the inconsistent findings of the associations
between obesity and urbanization.
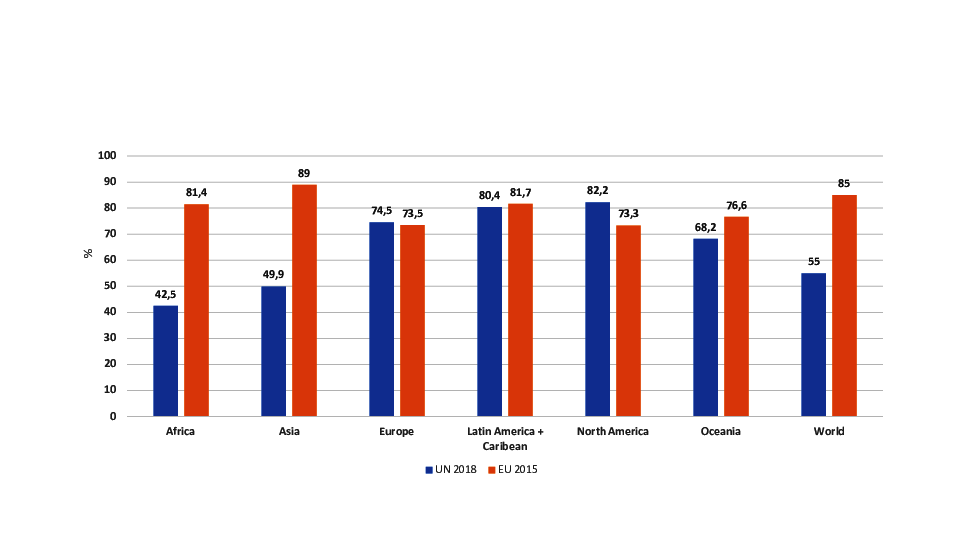
Figure 2 Urbanization world-wide in 2015 und 2018 – a comparison between the definition of
United Nations Organization and the definition of the European commission.
Urbanization from the viewpoint of evolutionary anthropology
From the perspective of evolutionary anthropology, urbanization or the trend towards
urban forms of settlement is a very recent phenomenon. More than 2 million years have
passed since the first appearance of the genus Homo (Antón and Snodgrass 2012). Anatomically modern Homo sapiens has been recorded for more than 150,000 years (Stringer 2016), but the first urban forms of life
appeared only around 10,000 years ago (Davis
1955; Wilkinson et al. 2014). The
environment in which the evolution to modern humans took place, the so-called "environment
of evolutionary adaptedness" (EEA) (Bowlby 1969),
therefore differed completely from current urban environments. Our ancestors followed a
hunter and gatherer lifestyle characterized by high mobility in small groups without
permanent homes. Group size seldom exceeded 100 people (Dunbar 1993), and the daily routine was determined by the search for food and
water. Living in crowded cities, overeating and lack of physical activity as a population
problem were equally unknown as the holding of domesticated animals with the exception of
dogs (Cohen et al. 2013).
As a result of the Neolithic transition, the earliest settlements known as “cities” –
such as Jericho, which is located in what is now the West Bank, or Catalhöyük in recent
Turkey – emerged around 10,000 years ago (Davis
1955; Mumford 1961; Maher et al. 2012; Wilkinson et al. 2014). The number of inhabitants did not exceed 3,000.
According to the current definition, both cities would correspond more to larger villages.
A higher number of inhabitants could not have been supported due to food supply problems,
because the technical possibilities in the Neolithic would not have enabled feeding a
larger population in a limited space. Technical innovations such as irrigation systems,
the use of the plow, or metallurgy made it possible to increase production and promoted
larger settlements that deserve the name city and comprised up to 15,000 inhabitants. Such
cities emerged in Egypt, Mesopotamia, China and India from 3,000 BC (Davis 1955). In the 2nd millennium BC, cities such as
Theben were assumed to already have over 100,000 inhabitants. Nonetheless, it was
difficult to cross the 200,000 inhabitants limit, as 50 to 90 farmers were still required
to produce food for one city dweller (Davis 1955;
Cohen et al. 2013). In the 5th
century BC, cities with over 100,000 inhabitants such as Athens, Carthage and Syracuse
emerged in the Mediterranean region. Rome was the first metropolis in history. Here,
improved agricultural technology, efficient traffic routes and highly developed
administration enabled the city dwellers to be fully supplied (Mumford 1961). On the other hand, a high incidence of infectious
diseases in urban habitats of the Roman Empire was reported for the 1st century
AD by Pliny the Elder in his Historia Naturalis and by von Galen in the 2nd
century AD (Scheidl 2010). With the exception of
Constantinople, ancient Rome represented the only megacity until London became the first
metropolis of modern times in the 19th century. Focusing on Europe, urban ways
of life established themselves from the High Medieval times, but the population remained
comparatively low. In the 14th century, Florence had around 90,000 inhabitants,
London around 30,000. The first major urbanization spurt came in the late 18th
and especially in the 19th century in the course of the Industrial Revolution
(Schott 2014). Starting in England, poverty
drove an increasing number of people from rural areas into the emerging industrial cities,
thus triggering urbanization. Around 1800 there were fewer than 50 cities with 100,000 or
more inhabitants worldwide, with only 1.7% of the world population living in cities with
more than 100,000 inhabitants, and 2.4% in cities with more than 20,000. In 1900 these
values were 5.5% and 9.2%, in 1950 13.1% and 20.9%, respectively (Davis 1955). In the last few decades this urbanization process has
reached the so-called emerging and developing countries and assumed unimagined
proportions.
Currently, we are confronted with the greatest wave of urbanization in human history. By
2030, 5 billion people are expected to live in urban conurbations and practice an urban
lifestyle. Urbanization is the result of the growth of existing cities, primarily through
rural-urban migration, the so-called physical urbanization. In turn, it also alters the
behavior of residents of rural regions in what is termed functional urbanization (Mumford 1961). This increase in the urban population
will primarily affect developing and emerging countries, which currently have an
urbanization rate of around 48%, whereas in the industrialized countries the proportion of
the urban population exceeded the 70% mark in 1990. In particular, this development will
present African and Asian countries with high population growth with unexpected challenges
in economic, ecological, but also social and health policy terms (Leon 2008; Bork et al.
2009).
The trend is towards megacities with more than 5 or even more than 10 million
inhabitants, depending on the definition, as well as polycentric agglomerations such as
the Pearl River Delta in southern China (Bork et al.
2009). There are currently more than 50 megacities worldwide, more than
two-thirds of which are in developing and emerging countries and are characterized by
barely manageable or controllable development. Examples include Istanbul (14 million),
Lagos (10 million), Sao Paolo (21 million), Cairo (17 million) Mexico City (20 million),
Kolkatta (14 million) or Mumbay (18.4 million), in which the living conditions can often
be described as catastrophic. This applies above all to the slum areas, which are
primarily inhabited by rural-urban migrants. These urban agglomerations are characterized
by overpopulation, environmental pollution, resource consumption, water scarcity, poor
hygienic conditions (Qian et al. 2001; Canfield et al. 2003; Schell 2014; Schell 2010;
Jaffar et al. 2017), social conflicts and the
resulting psychological stress (Calhoun 1962;
Dunbar 1993; Ramsden 2009; Logan and Jacka 2014;
Miller 2016) – all leading to increased disease
risks. At the same time, however, urban centers are characterized by better educational
and work opportunities as well as better access to health facilities (Bork et al. 2009).
Urban environments and parameters of human biology
Body height and growth patterns are widely used as biological welfare measurements and
public health indicators. Growth patterns and, ultimately, body height are influenced not
only by genetic disposition but also by environmental factors such as resource
availability, climate, nutrition, socioeconomic conditions as well as social status and
psychosocial factors (Bogin 2021; Schell et al. 2009). Furthermore, growth and body
height are associated with individual health status, but also with life circumstances and
social and economic conditions on the population level (Komlos 1994; Komlos 1998). Numerous
studies have examined the effects of the urban environment on growth patterns during the
subadult phase, body height and health (Tanner and
Eveleth 1976; Komlos 1986; Rona 2000; Martínez-Carrión and Moreno-Lázaro 2007). Growth inequalities and differences in
body height between inhabitants of urban and rural areas are of special interest. Up to
the Industrial Revolution, the differences between rural and urban populations in Europe
remained insignificant (Kaupová et al. 2013).
Thereafter, however, dramatic differences were reported in body height between rural and
urban populations, with a clear urban height penalty (Zehetmayer 2013). The body height of rural populations tended to exceed that of
urban ones. This urban penalty was mainly due to the low standard of sanitation, high
population density, high disease load and higher food prices in towns and emerging
Industrial cities (Martínez-Carrión and Moreno-Lázaro
2007). Such adverse urban environmental conditions impaired growth patterns and
ultimately led to a shorter stature among the urban population. Similar trends were
observed for the United States: during the 19th and early 20th
century, body heights and weights were lower in urban versus rural areas (Carson 2020). By the early 20th century,
however, this trend was almost universally reversed. Mortality rates fell and stature
height increased due to improved living conditions in European cities, including a
reduction of child labor, purification of the water supply, canalization and sanitation,
along with advances in the food supply, vaccination programs, medical care and higher
incomes (Schonfield et al. 1991; Komlos 1998). The body height of urban populations
exceeded those of their rural counterparts. Currently, rural-urban differences in body
height have diminished in most high-income countries. In middle- and low-income countries,
however, such differences still occur. In Venezuela, urban children were taller and
heavier than their rural counterparts. These differences were evident after age 2 and
puberty in boys and girls, and persisted into adulthood (Blanco et al. 1992). Major growth inequalities between urban and rural areas
have been reported in China over the past 40 years. Economic development and urbanization
decreased these differences in body height between children from rural and urban areas,
but new public health challenges emerged, in particular rising obesity rates (Zong et al. 2017; Hu et al. 2020).
Urban environments as health risks
Urbanization and urban environments are associated with various health risks. The high
population density represents ideal conditions for the spread of infectious diseases. This
is because enough hosts live in a confined space, enabling transmission through direct and
indirect contact. At the same time, high population densities also mean a problem for the
supply of pure drinking water, sufficient food, and waste disposal. The combination of
dense populations and poor hygiene predestines the occurrence of infectious diseases.
These patterns of infection incidence were also typical during plague pandemics several
centuries ago (Roberts and Lewis 2002), but even
today, infectious diseases were more common in urban areas. Beyond well-known infectious
diseases such as tuberculosis and influenza, new infectious diseases such as HIV/AIDS,
SARs, influenza, and COVID-19 also find an ideal biotope in overpopulated megacities
(Bork et al. 2009; Neiderud 2015).
Rapid urbanization has a clear impact on morbidity and mortality patterns (Vlahov et al. 2007; Leon 2008). This is unsurprising because changes in life style and
living conditions have always led to changes in the burden of illness. The negative impact
of urbanization on health started with the Neolithic transition and the associated first
epidemiological transition about 10,000 years ago (Armelagos et al. 2005), when the transition from an appropriative to a
productive subsistence forced people to give up a mobile way of life as hunters and
gatherers and to become sedentary farmers. The domestication of plants and animals, life
in village and later urban communities, and the changed food spectrum drastically altered
the burden of disease and reduced life expectancy. Although the main health problems of
these early stages of urbanization seem to be the rise of infectious diseases caused by
poor hygienic conditions and new emerging zoonoses, nutrition associated health problems
gain in importance. For the first time a double burden of malnutrition may be assumed. On
the one hand, the more one-sided and, due to crop failures, poor nutrition led to
starvation and malnutrition, on the other hand, reduced physical activity and diets rich
in carbohydrates and fat from domesticated animals may increase the risk of overweight for
the first time in human history (Cohen et al.
2013).
Malnutrition was still an important health hazard during the second epidemiological
transition, which took place during the Industrial Revolution in the late 18th
and early 19th centuries. There, the dramatic increase in population combined
with rapid urbanization and industrialization led to a dramatic deterioration in the
health situation in the emerging industrial cities (Roberts 2016). Beside the adverse effects of environmental pollution from
factories, overwork from toiling under inhumane conditions in industrial plants, and
catastrophic living and hygiene conditions on health and disease patterns, malnutrition
and associated diseases became an eminent problem. People in urban environments were no
longer able to produce their food by themselves, they had to buy it and spend a lot of
money to get enough food. Between 1780 and 1850 families in British industrialized cities
had to spend about 75% of their income on flood (Griffin
2018). Consequently, malnutrition and starvation were quite common. On the other
hand, since the industrial revolution refined grains and sugar have been consumed in huge
quantities, resulting in a frequent intake of high–glycemic index carbohydrates, which are
digested and absorbed quickly (Matthews 2012).
The double burden of malnutrition was omnipresent in the urban environment during the
Industrial Revolution.
The third epidemiological transition is currently taking place. The considerably improved
living conditions in the industrialized countries, combined with the enormous advances in
disease control and prevention, have led to completely new disease patterns in the last
few decades. Improvements in medicine, hygiene and vaccination programs pushed back
infectious diseases. This increased life expectancy, but the accompanying
hyperalimentation and rising obesity rates promoted so-called diseases of civilization or
non-communicable diseases such as cardiovascular diseases, metabolic disorders and cancer
(Pollard 2008).
Urban environment and obesity
Obesity rates are increasing worldwide, currently more rapidly in rural than in urban
areas (NCD Risk Factor Collaboration 2019; Mahase 2019). This increase in rural areas seems
confusing at a first glance because obesogenic environments are mainly found in urban
areas. One possible explanation may be, that rising obesity rates in poor rural areas
reflect nutrition and developmental assistance programs in low- and middle-income
countries, but also the expansion of an obesogenic environment from urban areas to rural
ones (Mou et al. 2013; Paciorek et al. 2013; Khan and
Kraemer 2014). Interestingly, the steadily increasing urbanization rates
unfortunately did not help reduce obesity rates in urban settlements. Even there, rising
rates of overweight and obesity represent a public health challenge. Another possible
explanation for this interesting trend of rising obesity rates in rural areas may be the
different definitions of rural and urban areas, which are used in different countries. As
pointed out above, there is no generally accepted definition what is a village, a city, a
town or what is rural, what is urban.
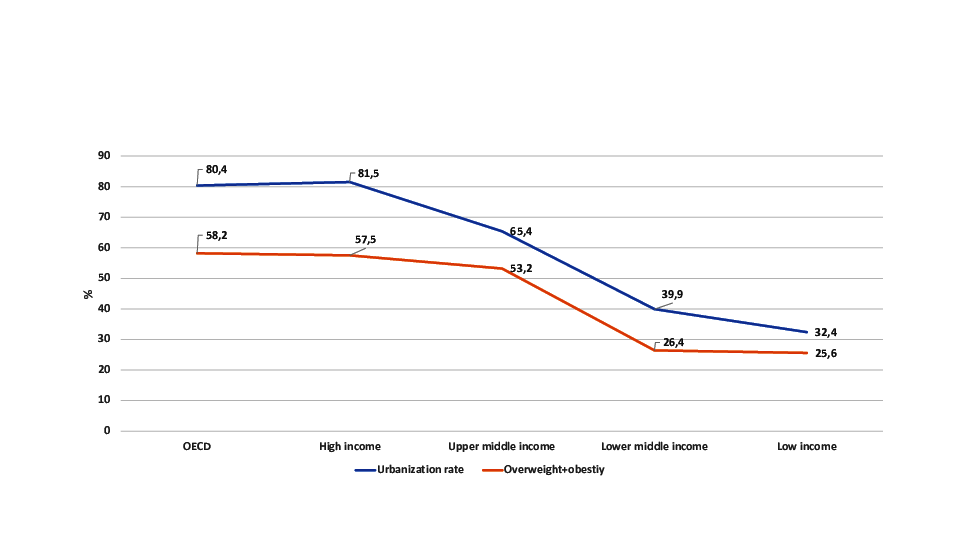
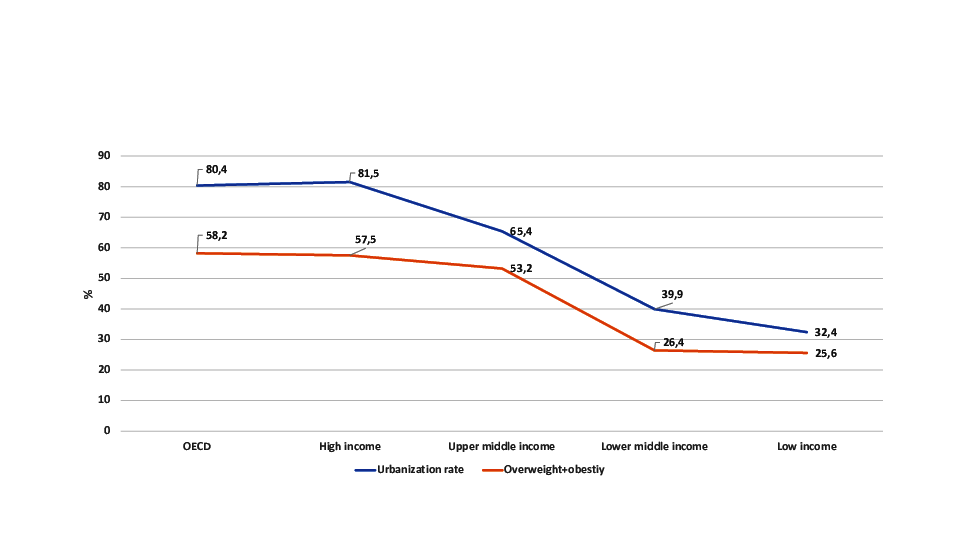
Figure 3 Overweight and obesity rates according to income regions according to the World
Bank (Shekar and Popkin 2020).
Figure 3 presents a comparison of urbanization
rate and overweight + obesity rate according to the World Bank income regions. This
comparison shows, that the urbanization rate as well as the overweight obesity rate among
adults drops down with decreasing income. The lower the urbanization rate, the lower is
the overweight+ obesity rate.
In order to discuss the effects of urban environment on overweight and obesity rates, it
is necessary to define an obesogenic environment. According to Swinburn et al. 1999, an “obesogenic environment” is “an environment
that promotes gaining weight and one that is not conducive to weight loss” within the home
or workplace. Thus, the obesogenic environment refers to one that helps, or contributes
to, obesity. But what are the characteristics of such an environment? The main
characteristics are conditions that reduce physical activity, a food environment that
promotes the availability and accessibility of cheap food rich in fat and sugar, and
social neighborhoods that are unsafe and stressful. Other typical obesogenic environments
are low-density areas with segregated land use, low connectivity and a high dependence of
car use, but also conditions which discourage walking, bicycling to schools or workplaces,
or outdoor physical activity during leisure. Note, however, that such conditions can
equally be found in nice middle-class suburban areas and in unsafe socioeconomically
disadvantaged neighborhoods (Congdon 2019).
Finally, a high density of fast food outlets, convenience stores offering processed
energy-dense food, as well as a stressful social environment and unsafe neighborhood that
address the hypothalamic-pituitary-adrenal axis and thus increase stress hormone levels
are typical of obesogenic environments (Congdon
2019).
For a long time, this type of environment was interpreted as being typical of
socioeconomically disadvantaged urban areas in high-income countries. Today, such
environmental conditions are increasingly found low- and middle-income countries, in
particular in rural areas which adopt these characteristics to interface with
modernization and globalization processes.
Overweight, obesity and associated metabolic diseases are typical of the
current third epidemiologic transition (Armelagos et al.
2005; Barrett et al. 1998). Obesogenic
environments are clearly the result of modernization processes, which started more than 50
years ago in high-income countries and now sprawl throughout the world. Technical advances
and modernization of lifestyle result in a marked transition in human life. The daily
energy effort to gather and prepare sufficient food is reduced to nearly zero because only
few individuals work in food production. Mechanized transportation, sedentary jobs and
labor-saving household technologies reduce physical activity too. At the same time, more
than enough energy-dense food, mainly consisting of sugar and fat, is easily available
(Popkin 2001; Popkin and Gordon-Larsen 2004; Lieberman
2006; Eaton and Konner 1985). Once a
problem of the industrialized world, globalization, modernization and urbanization now
promote obesogenic environments and enhance the risk of overweight and obesity in rural as
well as urban areas of developing countries. These include Indonesia (Nurwanti et al. 2019), India (Ebrahim et al. 2011), China (Dong
et al. 2019; Shen et al. 2019),
Guatemala (Groeneveld et al. 2007), or Peru
(Antiporta et al. 2016; Najera et al. 2019). In developed countries, poor neighborhoods, low
socioeconomic status and a background of migration are typical risk factors for overweight
and obesity among urban children and adults (Timmermans
et al. 2018; Ogden et al. 2018).
Today, in high-income countries such obesogenic environments are mainly found among lower
socioeconomic groups, characterized by low incomes, low educational levels and living in a
poor and unsafe neighborhood (Ball and Crawford
2005; Hook and Balistreri 2007; Faskunger et al. 2009; Wang and Beydoun 2007). These conditions are frequent in urban
environments. In middle- and low-income countries, in contrast, this relationship is
reversed. People of high socioeconomic status who underwent a rapid transition in
nutritional habits and general life style are more likely to be obese. In societies of
economic and nutritional transition, the paradox situation is that malnutrition and
obesity rise in parallel (Chatterjee 2002).
Moreover, numerous investigators have demonstrated that migrant status increases the risk
of overweight or obesity. This is true of rural-urban migrants in low-income countries, of
Hispanic immigrants in the United States (Kaplan et al.
2004), as well as of immigrants originating from Mediterranean countries or the
Middle East in Central and Northern Europe (Brussaard
et al. 2001; Kirchengast and Schober
2006; Misra and Ganda 2007; Wolin et al. 2009). Immigrant obesity is the result
of rapid modernization and a fast transition into an obesogenic environment.
An especially dramatic stress factor is transnational rural-urban migration. On the one
hand, urban conurbations are particularly attractive for migrants due to their mostly
multicultural character but also due to the diverse work and educational opportunities. On
the other hand, such transnational migration increases the risk of illness because
migration and integration into a new cultural environment are stress factors per se. In
addition, immigrants often have a lower social and socio-economic status than the guest
population and therefore live in cheaper and typically more polluted and disadvantaged
residential areas (Gushulak and MacPherson 2006).
Finally, a lower level of education and poor language skills impede access to medical
facilities (Carballo et al. 1998). Migration from
rural regions to an urban environment in another country therefore often represents a
double stress situation. Less daily physical activity and the availability of cheap,
sugar- and fat-rich food increase the risk of becoming obese. Thus, a significantly
increased risk of obesity and associated diseases was documented for Turkish and Indian
women who had migrated from rural regions in their home country to the city of Vienna
(Kilaf and Kirchengast 2011; Kirchengast et al. 2012). The obesity prevalence
among migrant women was significantly higher than that of women in their region of origin
as well as of Viennese women without a migration background. The main reasons for this are
probably changes in eating habits and a lack of exercise.
Overweight and obesity in Austria
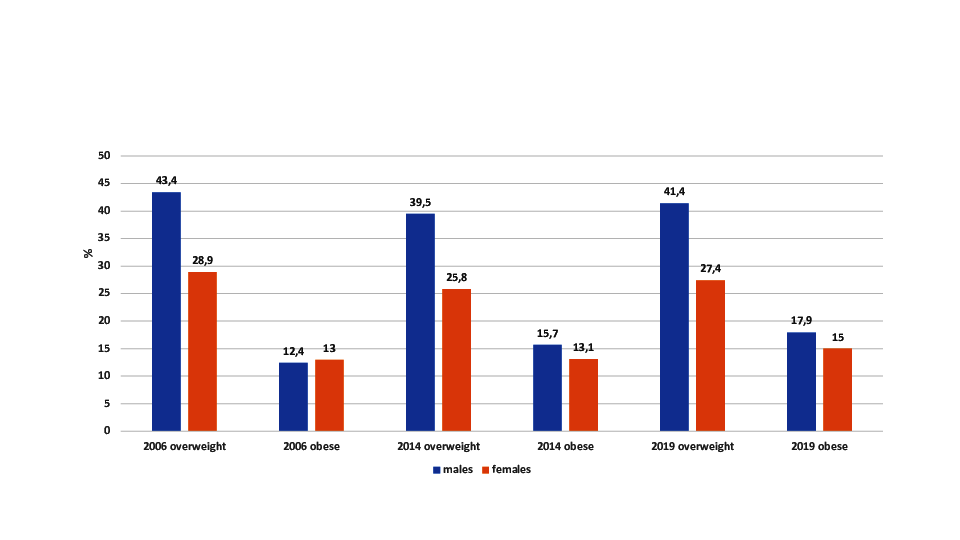
Overweight and obesity rates are high in Austria. As presented in Figure 4, during the last 15 years about 40% of adult males and
more than 25% of adult females were classified as overweight (BMI between 25.00 and
29.99kg/m2). Since 2006, the rates of obesity (BMI >30 kg/m2)
increased among males from 12.4% in 2014 to 17.9% in 2019. Among adult females, obesity
rates increased from 13% to 15% during the same period (Bundesanstalt Statistik Österreich 2019).
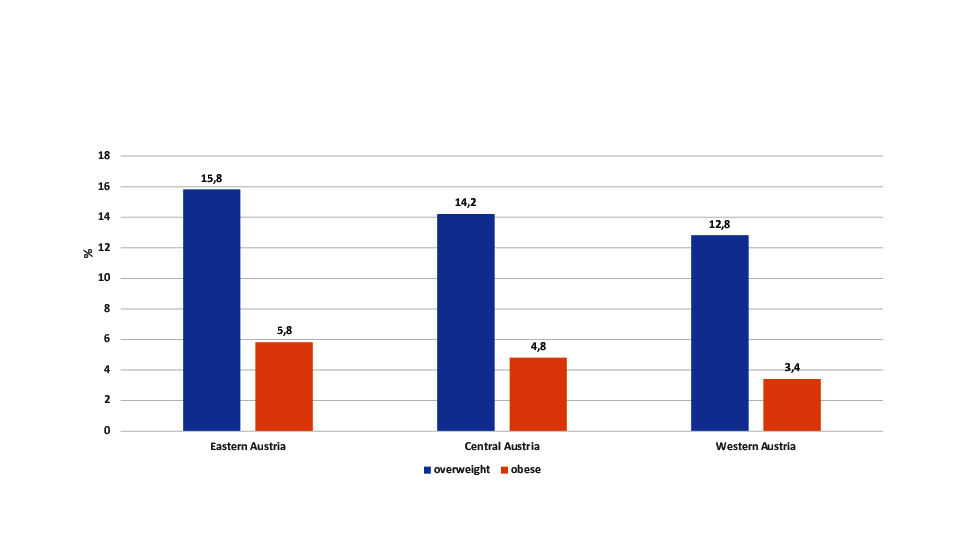
Furthermore, regional differences in the obesity prevalence are observable (Figure 5). The analysis of conscript data revealed lowest rates
of overweight and obesity in the rural Western areas of Austria and the highest overweight
and obesity rates for the more urbanized Eastern parts of Austria (Rami et al. 2004).
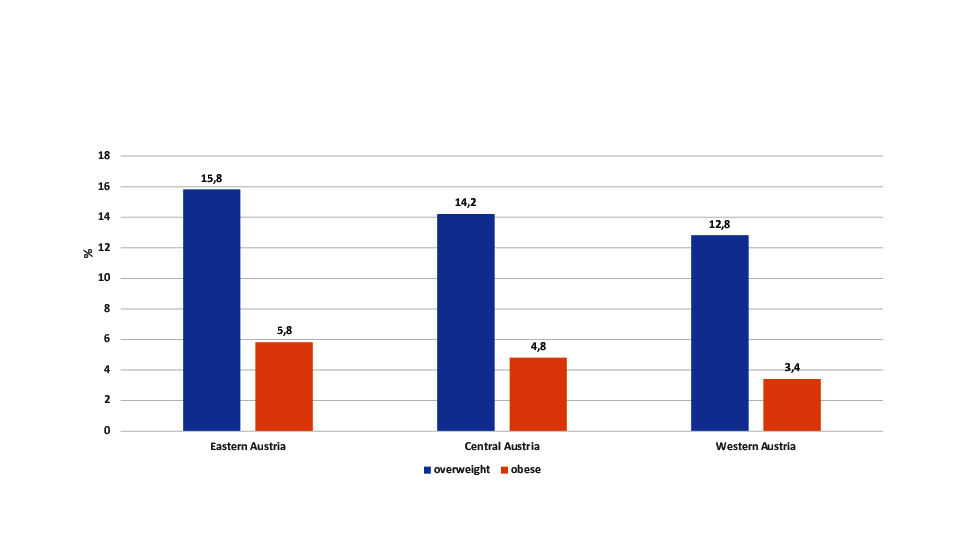
Figure 5 Overweight (BMI 25.00 to 29.99 kg/m2) and obesity (BMI > 30.00 kg/m2) among
Austrian conscripts according to Austrian region (Rami
et al. 2004).
Childhood overweight and obesity in Vienna, Austria
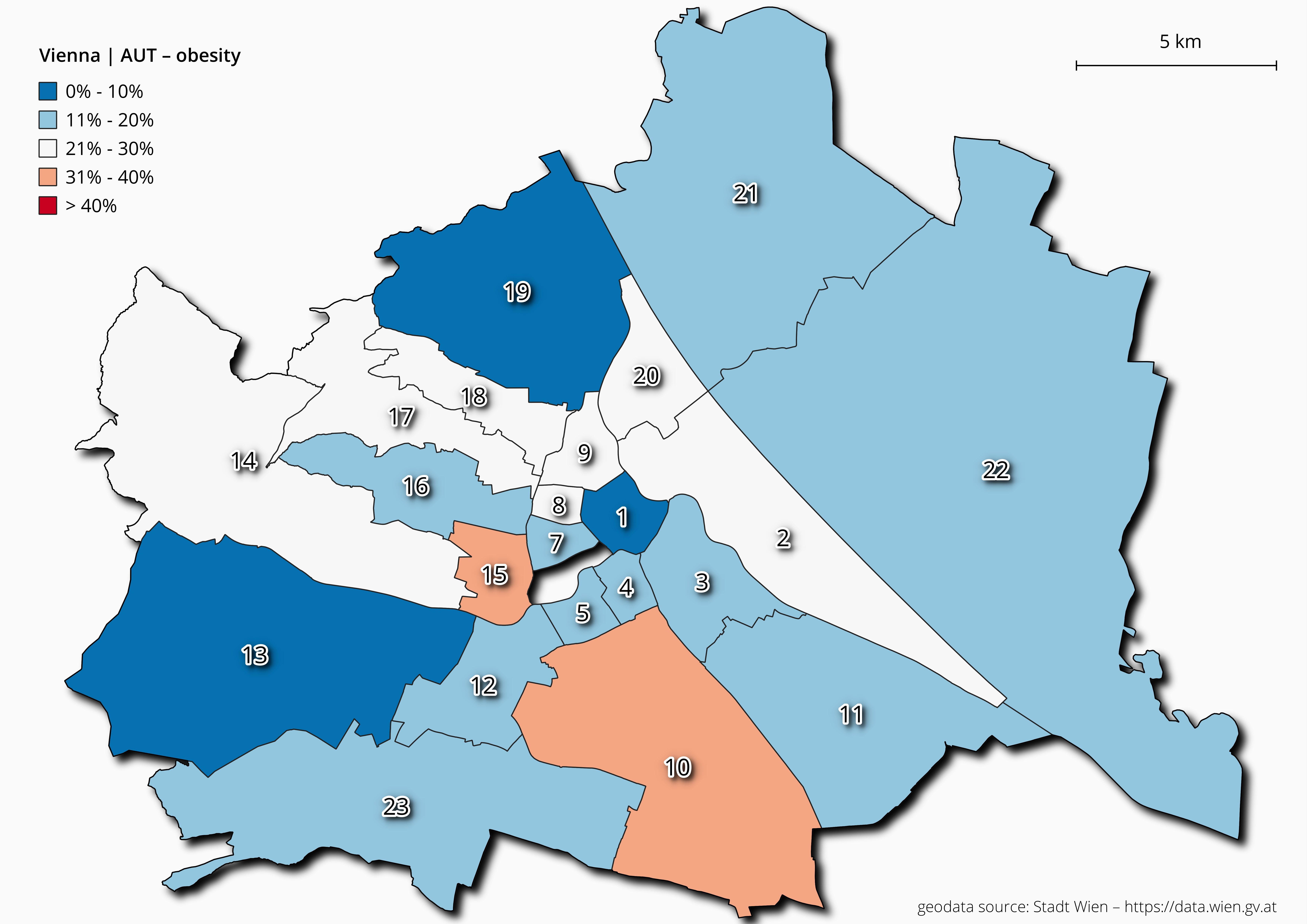
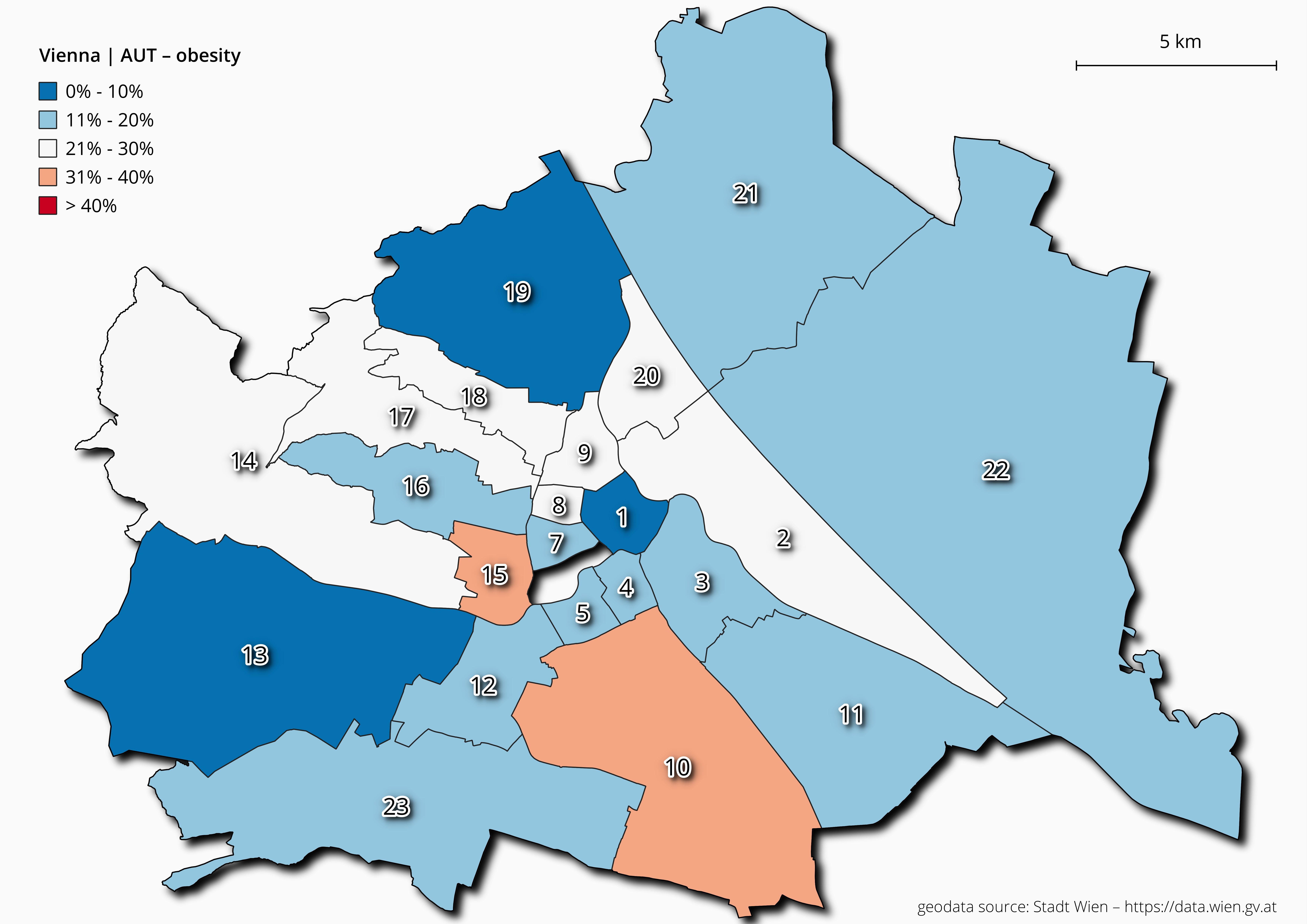
Figure 6 Overweight and obesity rates among 6-year-old children for each Viennese district.
A special problem represents the increasing rates of obesity and overweight among children
and adolescents (Ebbeling et al. 2002; Kimm and Obarzanek 2002; Wang and Lobstein 2006; Lasserre
et al. 2007; Han et al. 2010). On the one
hand obesity during childhood and adolescence has long-term health consequences (Must et al. 1992; McGee 2005), on the other hand childhood obesity predicts individual and global
economic problems (Withrow and Alter 2011). One
risk factor for obesity among children but also adults is a low socioeconomic status (Gnavi et al. 2000; Haas et al. 2003; Lissner et al. 2016;
Poulsen et al. 2018). Therefore, spatial
disparities in the prevalence of overweight and obesity in urban centers can be found (Kirchengast and Hagmann 2021).
As noted above, advancing urbanization is also associated with characteristic disease
risks, obesity being one example. Importantly, however, caution is advised against
generalizations, considering the current urbanizing world. Urban centers or cities are not
homogeneous environments. This also applies to the national and international comparison of
cities; even within a city, the individual districts differ in their economic, social and
ecological characteristics, and these are reflected in a regional variation of disease risks
even within a city. In Vienna, for example, life expectancy varies considerably between the
individual districts. In Vienna's upper-class districts such as the 13th or
19th districts, life expectancy is more than 7 years longer than in more
disadvantaged areas such as the 15th, 12th, 17th or
20th districts (Bachinger 2003; Bundesanstalt Statistik Österreich 2019), although the
spatial distance between the districts is quite small. These differences in life expectancy
depend mainly on the economic and social characteristics of the respective district.
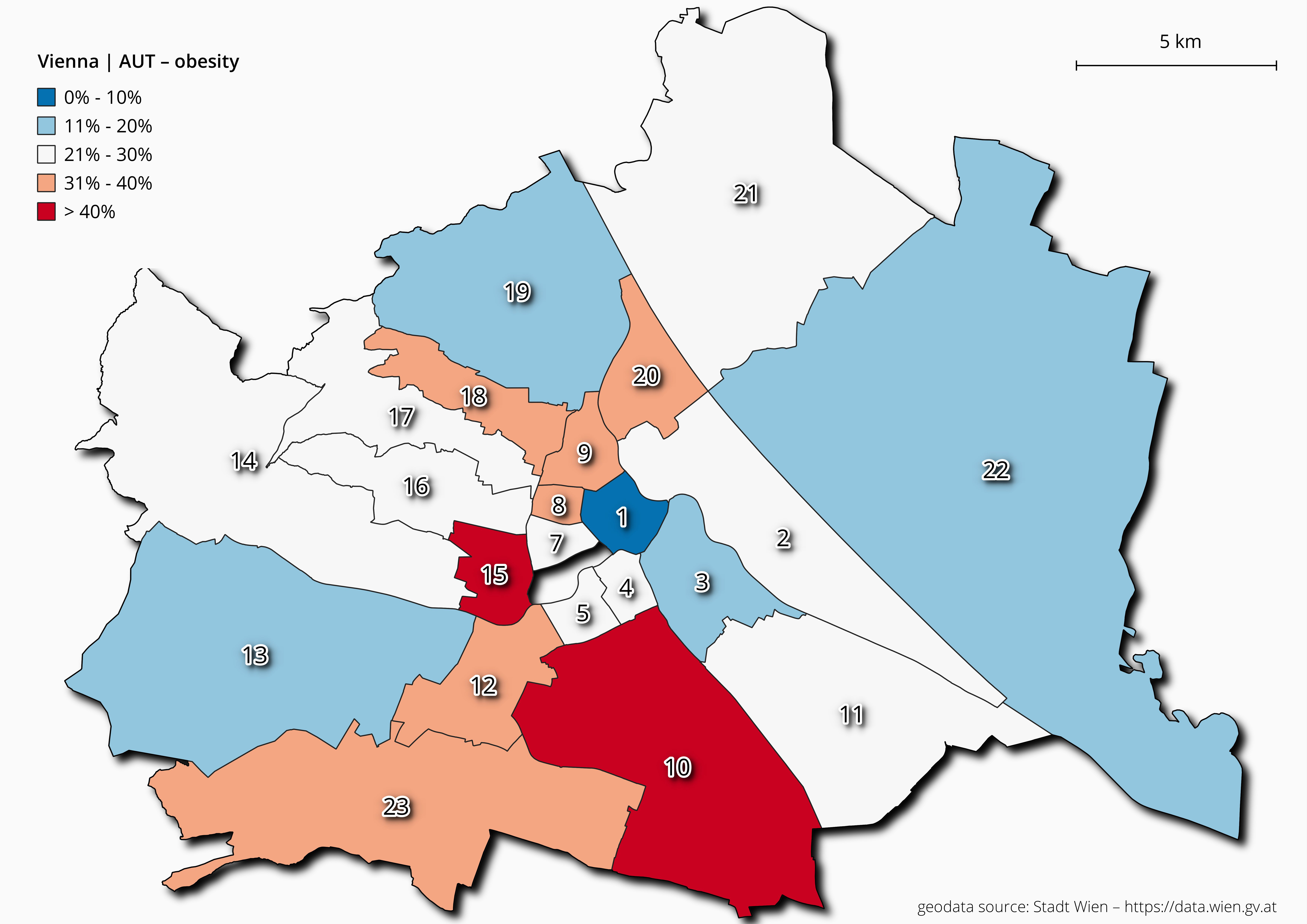
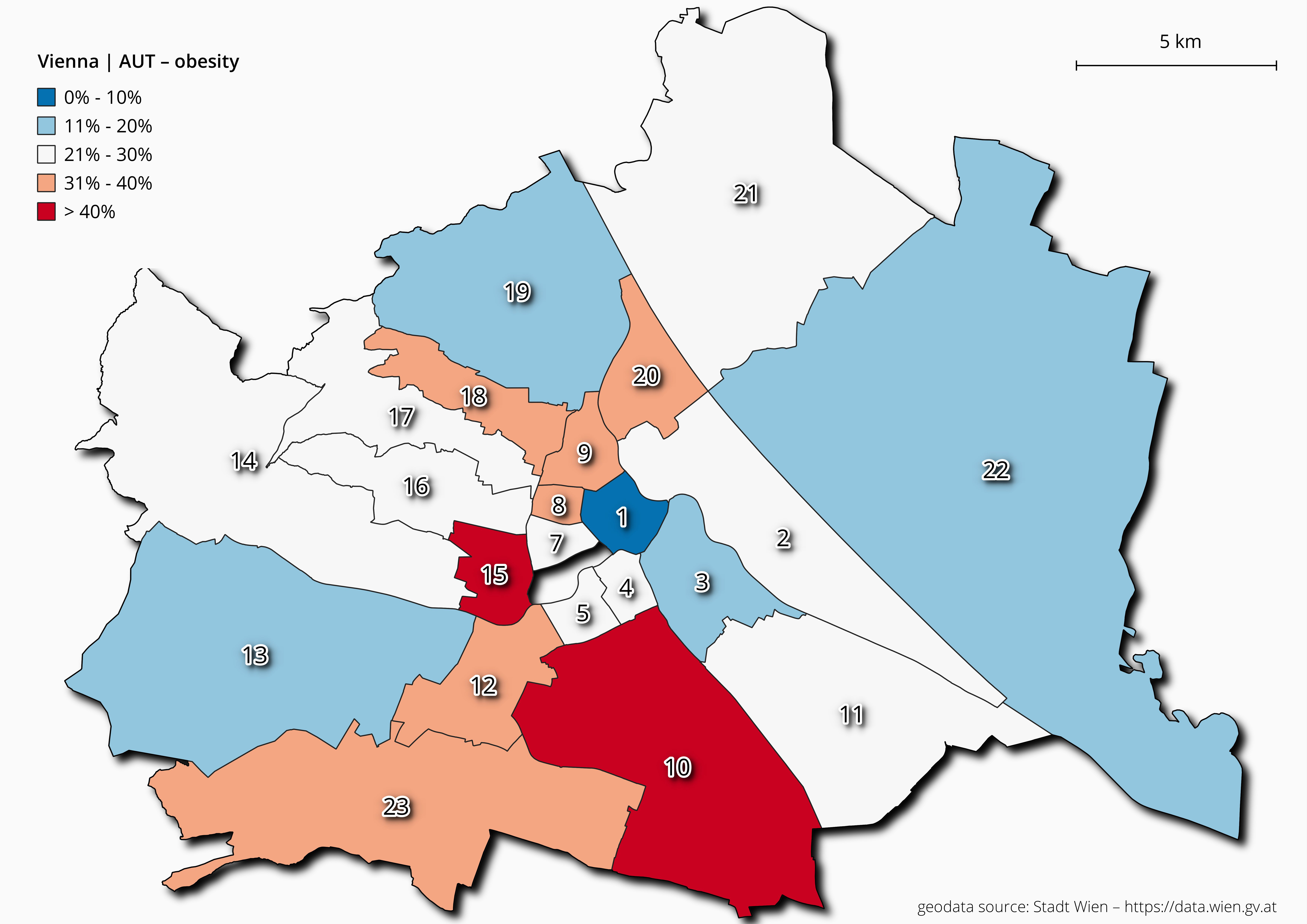
Figure 7 Overweight and obesity rates among 10-year-old children for each Viennese
district.
Equally, obesogenic environments differ between the individual districts. This is reflected
in the high prevalence of obesity among children and adolescents in socially disadvantaged
districts of Vienna (Kirchengast and Hagmann 2021).
In our study we analyzed a medical record-based dataset which was provided by the Viennese
school medical authority. Forty-four public secondary schools (two from each of the 23
districts of Vienna, with the exception of the sixth district) were randomly selected from
the Viennese school authority. In Austria, it is obligatory that – beside medical data – the
body height and body weight of all school children are collected by specially educated
personnel of the medical school authority. The data file including all information on body
heights and body weights are stored by the Viennese school medical office, to which we had
access. We analysed the data of 2,006 boys and 1,840 girls. Weight status was classified
according to the percentiles published by Kromeyer-Hausschild et al.(2001). These German charts are used because no
validated Austrian charts exist. A BMI(kg/m2) above the sex and age specific
90th percentile was defined as overweight, a BMI) above the age and sex
specific 97th percentile was defined as obese. In the present study, we included
all BMIs above the 90th percentile in one group, comprising obesity and
overweight. In order to compare the overweight and obesity rates between the individual
Viennese districts, we performed a spatial data analysis. We exported a data query of
classified percent shares for every Viennese district (except for the 6th
district, where no data was available for this study) from IBM SPSS in XLSX file
format. For the spatial data analysis, we loaded a structured table containing the
anthropological data and ESRI Shapefiles providing spatial information on Vienna (Stadt Wien 2011; Stadt Wien 2012) into the free and open-source geographic information system
software QGIS. As a coordinate reference system, we used EPSG:31256 MGI / Austria GK East.
For geostatistic analysis and mapping, we applied ‘natural breaks’ after Jenks (Jenks and Caspall 1971; Smith et al. 2020) to cluster the percent share of children per
district and then manually defined breaks to classify the anthropological dataset.
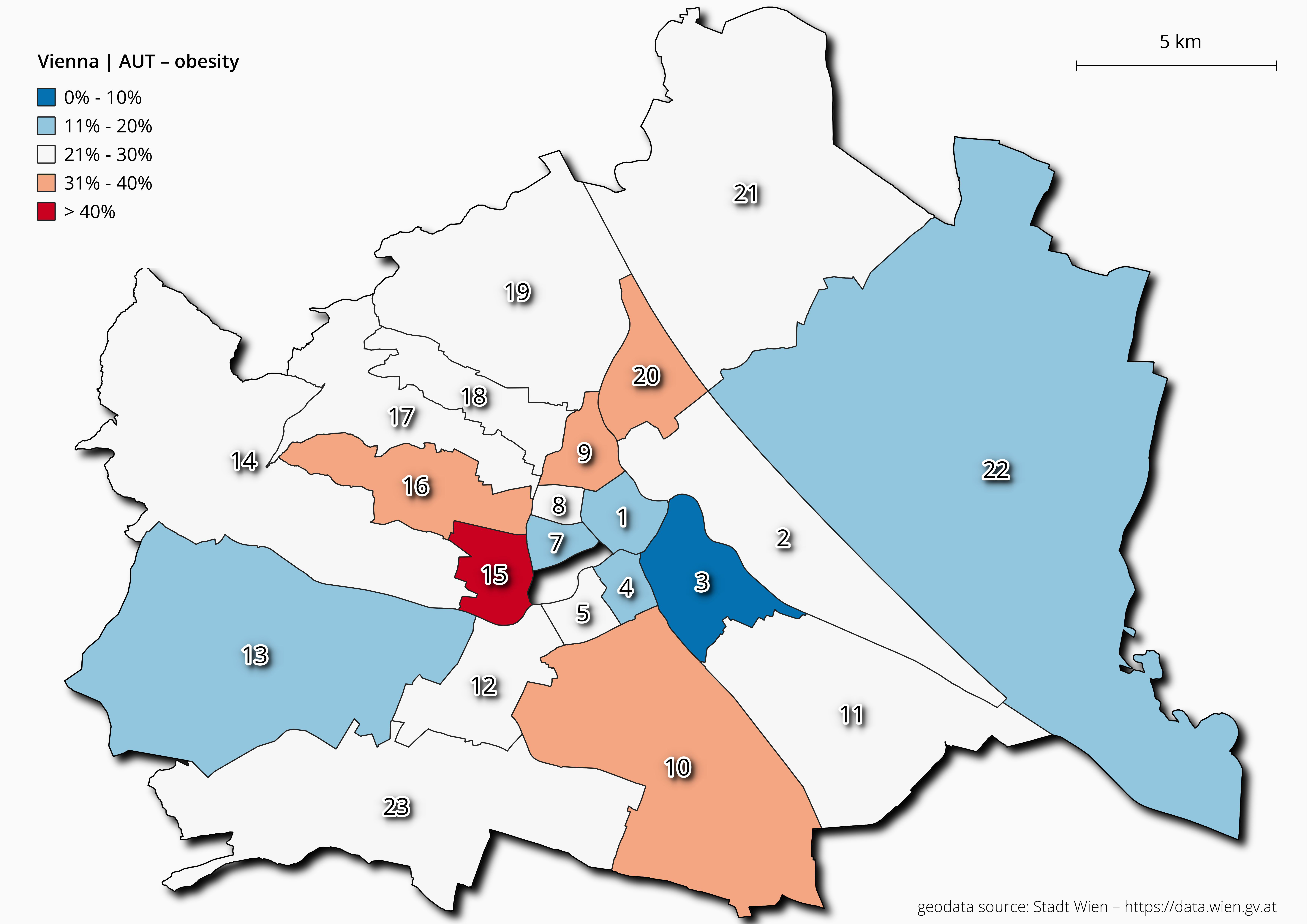
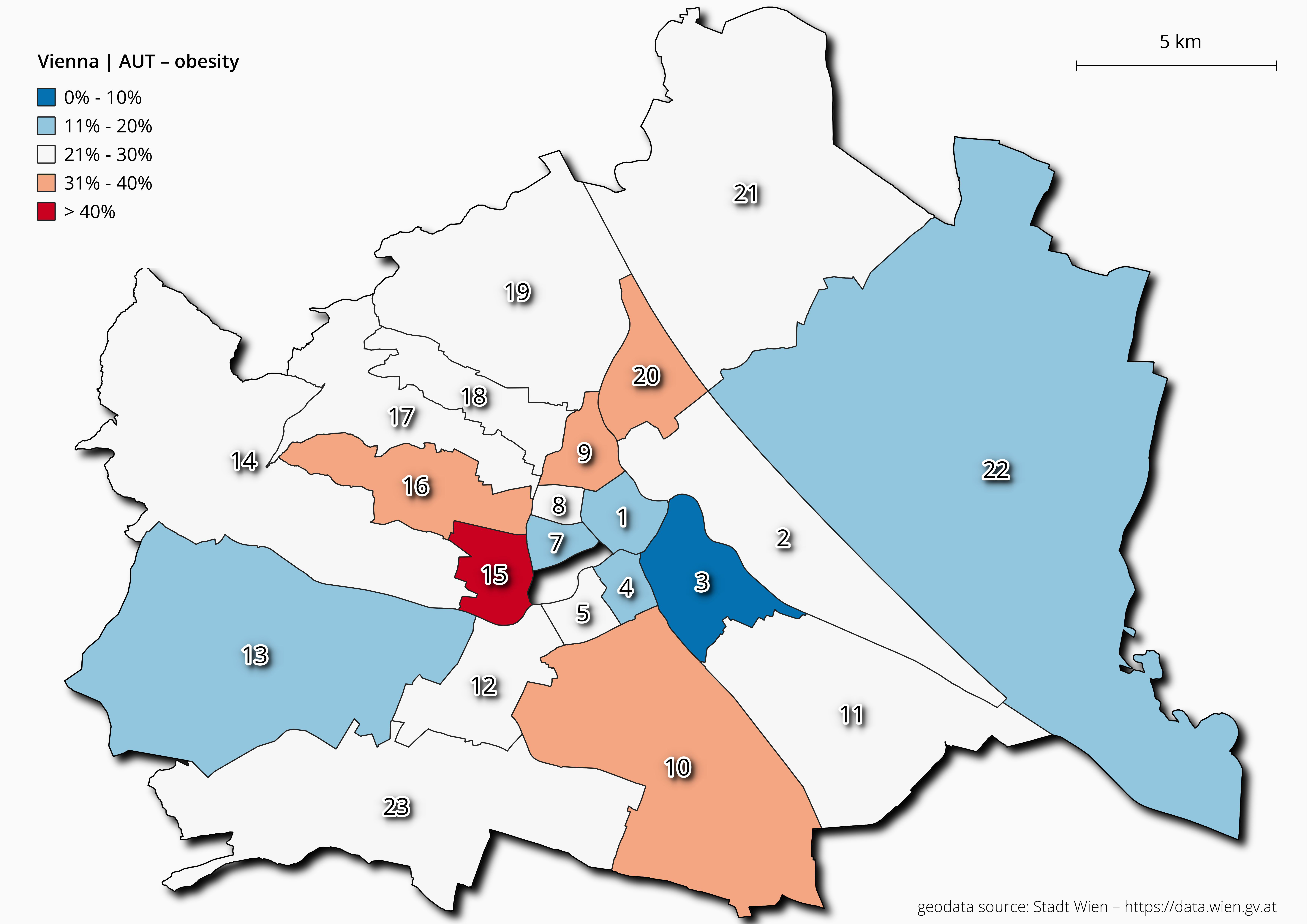
Figure 8 Overweight and obesity rates among 15-year-old adolescents for each Viennese
district.
As demonstrated in Figures 6, 7 and 8, the prevalence rates of
overweight and obesity differed markedly between the individual districts. The rates within
Vienna show spatial patterns that seem to correlate with the socioeconomic characteristics
of the districts. Among six-year-old children, the lowest rates of overweight and obesity
(<10%) were found in the 1st, 13th and 19th districts
(figure 6). These three districts are the most expensive areas of Vienna and are
characterized by a high quality of life, typical of inhabitants with a higher socioeconomic
status. In contrast, the highest prevalence (>30%) occurred in the 10th and
15th districts, both characterized by a lower socioeconomic status, poorer
living conditions and a high rate of inhabitants with a background of migration (Boztepe et al. 2019). At the age of 10 years, the
situation became worse for the children (figure 7).
With the exception of the 1st district, the prevalence rates of overweight and
obesity are above 10% in all Viennese districts. In the 15th and 10th
districts the prevalence rates increased to more than 40%. In six districts the rates were
between 30 to 40%. Among the age group 15 years, the 15th district still showed
the highest values (Figure 8). The analyses clearly
show marked spatial distribution patterns of overweight and obesity among Viennese school
children.
There is no doubt, that urban environments are not homogeneous areas, but we clearly see
that distinct differences between individual districts exists. Obesogenic environments are
mainly found in distinct districts, characterized by a high proportion of inhabitants with
lower educational level, lower socioeconomic status and a higher amount of inhabitants with
a background of migration such as the 10th and 15th district in
Vienna.
Conclusion
Urban centers are not only a place of innovation and economic and cultural diversity; they
are also living spaces that harbor a multitude of health risks. From the viewpoint of
evolutionary human biology, Homo sapiens is apparently still
insufficiently adapted to modern urban life. The 10,000 years of life experience in village
communities, the few thousand years in urban habitats, and the few decades of experience in
megacities were simply too short to enable adequate adaptation to these environmental
conditions. A special problem represents living in an obesogenic environment, typical of
today’s urban centers and urbanized rural areas. Urbanization or urban lifestyle and
increasing rates of overweight and obesity are interwoven. Therefore, both urbanization and
obesity are major topics of public health and human biology research.
References
Statistik Austria (Eds.) (2019). Demographic
Yearbook. Wien : Verlag Österreich GmbH.
Aggarwal, B./Jain, V. (2018). Obesity in children:
definition, etiology and approach. Indian Journal of Pediatrics 85 (6), 463–471.
https://doi.org/10.1007/s12098-017-2531-x.
Antiporta, D. A./Smeeth, L./Gilman, R. H./Miranda,
J. J. (2016). Length of urban residence and obesity among within-country rural-to-urban
Andean migrants. Public Health Nutrition 19 (7), 1270–1278. https://doi.org/10.1017/S1368980015002578.
Antón, S. C./Snodgrass, J. (2012). Origins and
evolution of genus homo. Current Anthropology 53 (S6), S479-S496. https://doi.org/10.1086/667692.
Armelagos, G. J./Brown, Peter J./Turner, B.
(2005). Evolutionary, historical and political economic perspectives on health and
disease. Social Science & Medicine (1982) 61 (4), 755–765. https://doi.org/10.1016/j.socscimed.2004.08.066.
Bachinger, E. (2003). Lebenserwartung und
Mortalität in Wien und Österreich ‐ Internationaler
Vergleich. Wien : Stadt Wien.
Ball, K./Crawford, D. (2005). Socioeconomic status
and weight change in adults: a review. Social Science & Medicine 60 (9), 1987–2010.
https://doi.org/10.1016/j.socscimed.2004.08.056.
Barrett, R./Kuzawa, Ch. W./McDade, T./Armelagos,
G. J. (1998). Emerging and re-emerging infectious diseases: The third epidemiologic
transition. Annual Review of Anthropology 27 (1), 247–271. https://doi.org/10.1146/annurev.anthro.27.1.247.
Blanco, M. L./Jimenez, M. L./Castellano, H. M.
(1992). Urban-rural differences in the growth status of Venezuelan children. American
Journal of Human Biology 4 (1), 105–113. https://doi.org/10.1002/ajhb.1310040113.
Blüher, M. (2019). Obesity: global epidemiology
and pathogenesis. Nature Reviews Endocrinology 15 (5), 288–298. https://doi.org/10.1038/s41574-019-0176-8.
Bogin, B. (2021). Patterns of Human Growth.
Cambridge : Cambridge University Press.
Bork, T./Butsch, C./Kraas, F./Kroll, M. (2009).
Megastädte - Neue Risiken für die Gesundheit. Deutsches Ärzteblatt 39 (106),
1877–1881.
Bowlby, J. (1969). Attachment. New York, Basic
Books.
Boztepe, K./Hammer, P./König, K. (2019).
Migrantinnen und Migranten in Wien 2019. Stadt Wien ‐
Integration und Diversität. Available online at https://www.digital.wienbibliothek.at/wbrup/content/titleinfo/3108775.
Brown, P. J. (1991). Culture and the evolution of
obesity. Human Nature 2 (1), 31–57. https://doi.org/10.1007/BF02692180.
Brussaard, J. H./van Erp-Baart, M. A./Brants, H.
A./Hulshof, K. F./Löwik, M. R. (2001). Nutrition and health among migrants in The
Netherlands. Public Health Nutrition 4 (2B), 659–664. https://doi.org/10.1079/PHN2001149.
Calhoun, J. B. (1962). Population density and
social pathology. Scientific American 206, 139–148. https://doi.org/10.1038/scientificamerican0262-139.
Canfield, R. L./Henderson, C. R./Cory-Slechta, D.
A./Cox, C./Jusko, T. A./Lanphear, B. P. (2003). Intellectual impairment in children with
blood lead concentrations below 10 microg per deciliter. The New England Journal of
Medicine 348 (16), 1517–1526. https://doi.org/10.1056/NEJMoa022848.
Carballo, M./Divino, J. J./Zeric, D. (1998).
Migration and health in the European Union. Tropical Medicine & International Health
3 (12), 936–944. https://doi.org/10.1046/j.1365-3156.1998.00337.x.
Carson, S. A. (2020). Biological differences
between late 19th and early 20th century urban and rural residence 2020. Available
online at https://www.cesifo.org/en/publikationen/2020/working-paper/biological-differences-between-late-19th-and-early-20th-century
(accessed 4/6/2021).
Caves, R. W. (2005). Encyclopedia of the city.
London : Routledge.
Chatterjee, P. (2002). India sees parallel rise in
malnutrition and obesity. The Lancet 360 (9349), 1948. https://doi.org/10.1016/S0140-6736(02)11943-X.
Chiurazzi, M./Cozzolino, M./Orsini, R. C./Di Maro,
Martina/Di Minno, M. N. D./Colantuoni, A. (2020). Impact of genetic variations and
epigenetic mechanisms on the risk of obesity. International Journal of Molecular
Sciences 21 (23). https://doi.org/10.3390/ijms21239035.
Chooi, Y. C./Ding, C./Magkos, F. (2019). The
epidemiology of obesity. Metabolism: Clinical and Experimental 92, 6–10. https://doi.org/10.1016/j.metabol.2018.09.005.
Cohen, M. N./Armelagos, G. J./Larsen, C. S. (Eds.)
(2013). Paleopathology at the origins of agriculture. Gainesville : University Press of
Florida.
Congdon, P. (2019). Obesity and urban
environments. International Journal of Environmental Research and Public Health 16 (3).
https://doi.org/10.3390/ijerph16030464.
Davis, K. (1955). The origin and growth of
urbanization in the world. American Journal of Sociology 60 (5), 429–437. https://doi.org/10.1086/221602.
Dong, Y./Ma, Y./Dong, B./Zou, Z./Hu, P./Wang,
Z./Yang, Y./Song, Y./Ma, J. (2019). Geographical variation and urban-rural disparity of
overweight and obesity in Chinese school-aged children between 2010 and 2014: two
successive national cross-sectional surveys. BMJ Open 9 (4), e025559. https://doi.org/10.1136/bmjopen-2018-025559.
Duignan, B. (2019). Encyclopædia Britannica.
Chicago : Encyclopædia Britannica Inc.
Dunbar, R. I. M. (1993). Coevolution of
neocortical size, group size and language in humans. Behavioral and Brain Sciences 16
(4), 681–694. https://doi.org/10.1017/S0140525X00032325.
Eaton, S. B./Konner, M. (1985). Paleolithic
nutrition. A consideration of its nature and current implications. The New England
Journal of Medicine 312 (5), 283–289. https://doi.org/10.1056/NEJM198501313120505.
Ebbeling, C. B./Pawlak, D. B./Ludwig, D. S.
(2002). Childhood obesity: public-health crisis, common sense cure. The Lancet 360
(9331), 473–482. Available online at https://www.academia.edu/2318105/Childhood_obesity_public_health_crisis_common_sense_cure.
Ebrahim, S./Kinra, S./Bowen, L./Andersen,
E./Ben-Shlomo, Y./Lyngdoh, T./Ramakrishnan, L./Ahuja, R. C./Joshi, P./Das, S. M./Mohan,
M./Smith, G. D./Prabhakaran, D./Reddy, K. S. (2011). Correction: The Effect of
rural-to-urban migration on obesity and diabetes in India: A cross-sectional study. PLoS
Medicine 8 (5). https://doi.org/10.1371/annotation/b1ecad56-652a-4a30-9920-26679d5a584a.
FAO (2008). The state of food insecurity in the
world. Roma 2008.
Faskunger, J./Eriksson, U./Johansson,
S.-E./Sundquist, K./Sundquist, J. (2009). Risk of obesity in immigrants compared with
Swedes in two deprived neighbourhoods. BMC public health 9, 304. https://doi.org/10.1186/1471-2458-9-304.
Florentino, R. F. (2002). The burden of obesity in
Asia: Challenges in assessment, prevention and management. Asia Pacific Journal of
Clinical Nutrition 11, S676-S680. https://doi.org/10.1046/j.1440-6047.11.s8.4.x.
Ford, E. S./Mokdad, A. H. (2008). Epidemiology of
obesity in the western hemisphere. The Journal of Clinical Endocrinology and Metabolism
93 (11 Suppl 1), S1-8. https://doi.org/10.1210/jc.2008-1356.
Gnavi, R./Spagnoli, T. D./Galotto, C./Pugliese,
E./Carta, A./Cesari, L. (2000). Socioeconomic status, overweight and obesity in
prepuberal children: a study in an area of Northern Italy. European Journal of
Epidemiology 16 (9), 797–803. https://doi.org/10.1023/A:1007645703292.
Griffin, E. (2018). Diets, hunger and living
standards during the british industrial revolution. Past & Present 239 (1), 71–111.
https://doi.org/10.1093/pastj/gtx061.
Groeneveld, I. F./Solomons, N. W./Doak, C. M.
(2007). Nutritional status of urban schoolchildren of high and low socioeconomic status
in Quetzaltenango, Guatemala. Revista Panamericana de Salud Publica - Pan American
Journal of Public Health 22 (3), 169–177. https://doi.org/10.1590/s1020-49892007000800003.
Gushulak, B. D./MacPherson, D. W. (2006). The
basic principles of migration health: population mobility and gaps in disease
prevalence. Emerging Themes in Epidemiology 3, 3. https://doi.org/10.1186/1742-7622-3-3.
Haas, J. S./Lee, L. B./Kaplan, C. P./Sonneborn,
D./Phillips, K. A./Liang, S.-Y. (2003). The association of race, socioeconomic status,
and health insurance status with the prevalence of overweight among children and
adolescents. American Journal of Public Health 93 (12), 2105–2110. https://doi.org/10.2105/ajph.93.12.2105.
Han, J. C./Lawlor, D. A./Kimm, S. Y. S. (2010).
Childhood obesity. The Lancet 375 (9727), 1737–1748. https://doi.org/10.1016/S0140-6736(10)60171-7.
Haslam, D. (2007). Obesity: a medical history.
Obesity Reviews 8 Suppl 1, 31–36. https://doi.org/10.1111/j.1467-789X.2007.00314.x.
Hook, J. van/Balistreri, K. S. (2007). Immigrant
generation, socioeconomic status, and economic development of countries of origin: a
longitudinal study of body mass index among children. Social Science & Medicine 65
(5), 976–989. https://doi.org/10.1016/j.socscimed.2007.04.032.
Hossain, P./Kawar, B./El Nahas, M. (2007). Obesity
and diabetes in the developing world‐a growing
challenge. The New England Journal of Medicine 356 (3), 213–215. https://doi.org/10.1056/NEJMp068177.
Hu, Yan/Lin, Weiqun/Tan, Xuying/Liu, Yu/Wen,
Yuqi/Xing, Yanfei/Ma, Ying/Liu, Huiyan/Song, Yanyan/Liang, Jingjing/Lam, Kin Bong
Hubert/Lin, Suifang (2020). Trends in urban/rural inequalities in physical growth among
Chinese children over three decades of urbanization in Guangzhou: 1985-2015. BMC Public
Health 20 (1), 1190. https://doi.org/10.1186/s12889-020-09239-7.
Jaffar, S. T. A./Chen, L.-Z./Younas, H./Ahmad, N.
(2017). Heavy metals pollution assessment in correlation with magnetic susceptibility in
topsoils of Shanghai. Environmental Earth Sciences 76 (7). https://doi.org/10.1007/s12665-017-6598-5.
Jenks, G. F./Caspall, F. C. (1971). Error on
choroplethic maps: Definition, measurement, reduction. Annals of the Association of
American Geographers 61 (2), 217–244. https://doi.org/10.1111/j.1467-8306.1971.tb00779.x.
Kaplan, M. S./Huguet, N./Newsom, J. T./McFarland,
B. H. (2004). The association between length of residence and obesity among Hispanic
immigrants. American Journal of Preventive Medicine 27 (4), 323–326. https://doi.org/10.1016/j.amepre.2004.07.005.
Kaupová, S./Brůzek, J./Velemínský, P./Cerníková,
A. (2013). Urban-rural differences in stature in the population of medieval Bohemia.
Anthropologischer Anzeiger 70 (1), 43–55. https://doi.org/10.1127/0003-5548/2012/0276.
Khan, M. M. H./Kraemer, A. (2014). Are rural-urban
migrants living in urban slums more vulnerable in terms of housing, health knowledge,
smoking, mental health and general health? International Journal of Social Welfare 23
(4), 373–383. https://doi.org/10.1111/ijsw.12053.
Kilaf, E./Kirchengast, S. (2011). Socio-economic
position and obesity among Turkish migrant women in Vienna, Austria. Journal of Life
Sciences 3 (2), 107–116. https://doi.org/10.1080/09751270.2011.11885177.
Kimm, S. Y. S./Obarzanek, E. (2002). Childhood
obesity: a new pandemic of the new millennium. Pediatrics 110 (5), 1003–1007. https://doi.org/10.1542/peds.110.5.1003.
Kirchengast, S./Hagmann, D. (2021). Spatial
disparity in the prevalence of childhood obesity in Vienna. 2021: in
prep.
Kirchengast, S./Schober, E. (2006). To be an
immigrant: a risk factor for developing overweight and obesity during childhood and
adolescence? Journal of Biosocial Science 38 (5), 695–705. https://doi.org/10.1017/S0021932005027094.
Kirchengast, S./Singh, M./Kilaf, E. (2012).
Obesity prevalence and socioeconomic position among two different groups of immigrant
women in Vienna, Austria. In: M. P. Martinez/H. Robinson (Eds.). Obesity and Weight
Management: Challenges, Practices and Health Implications. NOVA Publisher,
71–92.
Komlos, J. (1986). Patterns of children’s growth
in east-central Europe in the eighteenth century. Annals of Human Biology 13 (1), 33–48.
https://doi.org/10.1080/03014468600008181.
Komlos, J. (Ed.) (1994). Stature, living
standards, and economic development: Essays in Anthropometric History. Chicago : Univ.
of Chicago Press.
Komlos, J. (Ed.) (1998). The biological standard
of living in comparative perspective: Contributions to the conference held in Munich
January 18-22, 1997, for the XIIth Congress of the International Economic History
Association. Stuttgart : Steiner.
Kromeyer-Hausschild, K./Wabitsch, M./Kunze,
D./Geller, F./Geiß, H. C./Hesse, V./von Hippel, A./Jäger, U./Korte, W./Menner,
K./Müller, G./Müller, J. M./Niemann-Pilatus, A./Remer, T./Schäfer, F./Wittchen, H.
U./Zabransky, S./Zellner, K./Ziegler, A./Hebebrand, J. (2001). Perzentile für den
Bodymass Index für das Kindes- und Jugendalter unter Heranziehung verschiedener
deutscher Stichproben. Monatsschrift Kinderheilkunde (149), 807–818.
Lasserre, A. M./Chiolero, A./Paccaud, F./Bovet, P.
(2007). Worldwide trends in childhood obesity. Swiss Medical Weekly 137 (9-10),
157–158.
Leon, D. A. (2008). Cities, urbanization and
health. International Journal of Epidemiology 37 (1), 4–8. https://doi.org/10.1093/ije/dym271.
Lieberman, L. S. (2006). Evolutionary and
anthropological perspectives on optimal foraging in obesogenic environments. Appetite 47
(1), 3–9. https://doi.org/10.1016/j.appet.2006.02.011.
Lissner, L./Wijnhoven, T. M. A./Mehlig,
K./Sjöberg, A./Kunesova, M./Yngve, A./Petrauskiene, A./Duleva, V./Rito, A. I./Breda, J.
(2016). Socioeconomic inequalities in childhood overweight: heterogeneity across five
countries in the WHO European Childhood Obesity Surveillance Initiative (COSI-2008).
International Journal of Obesity 40 (5), 796–802. https://doi.org/10.1038/ijo.2016.12.
Logan, A. C./Jacka, F. N. (2014). Nutritional
psychiatry research: an emerging discipline and its intersection with global
urbanization, environmental challenges and the evolutionary mismatch. Journal of
Physiological Anthropology 33, 22. https://doi.org/10.1186/1880-6805-33-22.
Mahase, E. (2019). Obesity rates are increasing
more rapidly in rural areas than in cities. BMJ 365, l2088. https://doi.org/10.1136/bmj.l2088.
Maher, L. A./Richter, T./Macdonald, D./Jones, M.
D./Martin, L./Stock, J. T. (2012). Twenty thousand-year-old huts at a hunter-gatherer
settlement in eastern Jordan. PloS One 7 (2), e31447. https://doi.org/10.1371/journal.pone.0031447.
Martínez-Carrión, J.-M./Moreno-Lázaro, J. (2007).
Was there an urban height penalty in Spain, 1840-1913? Economics and Human Biology 5
(1), 144–164. https://doi.org/10.1016/j.ehb.2006.09.001.
Matthews, C. M. (2012). Exploring the obesity
epidemic. Proceedings (Baylor University. Medical Center) 25 (3), 276–277. https://doi.org/10.1080/08998280.2012.11928848.
McGee, D. L. (2005). Body mass index and
mortality: a meta-analysis based on person-level data from twenty-six observational
studies. Annals of Epidemiology 15 (2), 87–97. https://doi.org/10.1016/j.annepidem.2004.05.012.
Miller, G. (2016). Roots of the urban mind.
Science 352 (6288), 908–911. https://doi.org/10.1126/science.352.6288.908.
Misra, A./Ganda, O. P. (2007). Migration and its
impact on adiposity and type 2 diabetes. Nutrition 23 (9), 696–708. https://doi.org/10.1016/j.nut.2007.06.008.
Mou, J./Griffiths, S. M./Fong, H./Dawes, M. G.
(2013). Health of China’s rural-urban migrants and their families: a review of
literature from 2000 to 2012. British Medical Bulletin 106, 19–43. https://doi.org/10.1093/bmb/ldt016.
Mumford, L. (1961). The city in history: Its
origins, its transformations, and its prospects. San Diego and New York and London,
Harcourt Inc.
Must, A./Jacques, P. F./Dallal, G. E./Bajema, C.
J./Dietz, W. H. (1992). Long-term morbidity and mortality of overweight adolescents. A
follow-up of the Harvard Growth Study of 1922 to 1935. The New England Journal of
Medicine 327 (19), 1350–1355. https://doi.org/10.1056/NEJM199211053271904.
Najera, H./Nandy, S./Carrillo-Larco, R.
M./Miranda, J. J. (2019). Within-country migration and obesity dynamics: analysis of
94,783 women from the Peruvian demographic and health surveys. BMC public health 19 (1),
263. https://doi.org/10.1186/s12889-019-6586-7.
NCD Risk Factor Collaboration (2019). Rising rural
body-mass index is the main driver of the global obesity epidemic in adults. Nature 569
(7755), 260–264. https://doi.org/10.1038/s41586-019-1171-x.
Neiderud, C.-J. (2015). How urbanization affects
the epidemiology of emerging infectious diseases. Infection Ecology & Epidemiology
5, 27060. https://doi.org/10.3402/iee.v5.27060.
Nurwanti, E./Hadi, H./Chang, J.-S./Chao, J.
C.-J./Paramashanti, B. A./Gittelsohn, J./Bai, C.-H. (2019). Rural-urban differences in
dietary Behavior and obesity: Results of the Riskesdas study in 10-18-year-old
indonesian children and adolescents. Nutrients 11 (11). https://doi.org/10.3390/nu11112813.
Ogden, C. L./Fryar, C. D./Hales, C. M./Carroll, M.
D./Aoki, Y./Freedman, D. S. (2018). Differences in obesity prevalence by demographics
and urbanization in US children and adolescents, 2013-2016. JAMA 319 (23), 2410–2418.
https://doi.org/10.1001/jama.2018.5158.
Paciorek, C. J./Stevens, G. A./Finucane, M.
M./Ezzati, M. (2013). Children’s height and weight in rural and urban populations in
low-income and middle-income countries: a systematic analysis of
population-representative data. The Lancet Global Health 1 (5), e300-e309. https://doi.org/10.1016/S2214-109X(13)70109-8.
Pijl, H. (2011). Obesity: evolution of a symptom
of affluence. The Netherlands Journal of Medicine 69 (4), 159–166.
Pollard, T. M. (2008). Western diseases: An
evolutionary perspective. Cambridge : Cambridge University Press.
Popkin, B. M. (2001). The nutrition transition and
obesity in the developing world. The Journal of Nutrition 131 (3), 871S-873S. https://doi.org/10.1093/jn/131.3.871S.
Popkin, B. M. (2003). The nutrition transition in
the developing world. Development Policy Review 21 (5-6), 581–597. https://doi.org/10.1111/j.1467-8659.2003.00225.x.
Popkin, B. M./Gordon-Larsen, P. (2004). The
nutrition transition: worldwide obesity dynamics and their determinants. International
Journal of Obesity and related Metabolic Disorders 28 Suppl 3, S2-9. https://doi.org/10.1038/sj.ijo.0802804.
Popkin, B. M./Udry, J. R. (1998). Adolescent
obesity increases significantly in second and third generation U.S. immigrants: the
national longitudinal study of adolescent health. The Journal of Nutrition 128 (4),
701–706. https://doi.org/10.1093/jn/128.4.701.
Poston, W. S. C./Foreyt, J. P. (1999). Obesity is
an environmental issue. Atherosclerosis 146 (2), 201–209. https://doi.org/10.1016/s0021-9150(99)00258-0.
Poulsen, P. H./Biering, K./Winding, T. N./Nohr, E.
A./Andersen, J. H. (2018). How does childhood socioeconomic position affect overweight
and obesity in adolescence and early adulthood: a longitudinal study. BMC obesity 5, 34.
https://doi.org/10.1186/s40608-018-0210-8.
Qian, Z./Zhang, J./Wei, F./Wilson, W. E./Chapman,
R. S. (2001). Long-term ambient air pollution levels in four Chinese cities: inter-city
and intra-city concentration gradients for epidemiological studies. Journal of exposure
analysis and environmental epidemiology 11 (5), 341–351. https://doi.org/10.1038/sj.jea.7500170.
Rami, B./Schober, E./Kirchengast, S./Waldhör,
T./Sefranek, R. (2004). Prevalence of overweight and obesity in male adolescents in
Austria between 1985 and 2000. A population based study. Journal of Pediatric
Endocrinology & Metabolism 17 (1), 67–72. https://doi.org/10.1515/jpem.2004.17.1.67.
Ramsden, E. (2009). The urban animal: population
density and social pathology in rodents and humans. Bulletin of the World Health
Organization 87 (2), 82. https://doi.org/10.2471/BLT.09.062836.
Roberts, C. A. (2016). Palaeopathology and its
relevance to understanding health and disease today: the impact of the environment on
health, past and present. Anthropological Review 79 (1), 1–16. https://doi.org/10.1515/anre-2016-0001.
Roberts, C. A./Lewis, M. E. (2002). Ecology and
infectious disease in Britain from prehistory to the present: The Case of Respiratory
infections. Biennial Books of EEA (2), 179–192.
Rona, R. J. (2000). The impact of the environment
on height in Europe: conceptual and theoretical considerations. Annals of human biology
27 (2), 111–126. https://doi.org/10.1080/030144600282235.
Scheidl, W. (2010). Disease and death in the
ancient city of Rome. In: P. Erdkamp (Ed.). The Companion to Ancient Rome. Cambridge
University Press.
Schell, L. M. (2010). Industrial polluntants and
human evolution. In: M. P. Mühlenheim (Ed.). Human Evolutionary Biology. Cambridge
University Press, 566–580.
Schell, L. M. (2014). Culture, urbanism and
changing human biology. Global Bioethics - Problemi di bioetica 25 (2), 147–154.
https://doi.org/10.1080/11287462.2014.897070.
Schell, L. M./Gallo, M. V./Ravenscroft, J. (2009).
Environmental influences on human growth and development: historical review and case
study of contemporary influences. Annals of human biology 36 (5), 459–477. https://doi.org/10.1080/03014460903067159.
Schonfield, R./Reher, D./Bideau, A. (1991). The
decline of mortality in Europe. Oxford, Clarendon Press Oxford.
Schott, D. (2014). Europäische Urbanisierung (1000
- 2000): Eine umwelthistorische Einführung. Köln, Böhlau.
Shekar, M./Popkin, B. (Eds.) (2020). Obesity:
Health and economic consequences of an impending global challenge. Washington,
DC.
Shen, C./Zhou, Z./Lai, S./Tao, X./Zhao, D./Dong,
W./Li, D./Lan, X./Gao, J. (2019). Urban-rural-specific trend in prevalence of general
and central obesity, and association with hypertension in Chinese adults, aged 18-65
years. BMC public health 19 (1), 661. https://doi.org/10.1186/s12889-019-7018-4.
Smith, M. J. de/Goodchild, M. F./Longley, P.
(2020). Geospatial analysis: A comprehensive guide to principles, techniques and
software tools. 6th ed. Leicester, Matador.
Spinelli, A./Buoncristiano, M./Kovacs, V.
A./Yngve, A./Spiroski, I./Obreja, G./Starc, G./Pérez, N./Rito, A. I./Kunešová,
M./Sant’Angelo, V. F./Meisfjord, J./Bergh, I. H./Kelleher, C./Yardim, N./Pudule,
I./Petrauskiene, A./Duleva, V./Sjöberg, A./Gualtieri, A./Hassapidou, M./Hyska,
J./Burazeri, G./Petrescu, C. H./Heinen, M./Takacs, H./Zamrazilová, H./Bosi, T.
B./Sacchini, E./Pagkalos, I./Cucu, A./Nardone, P./Gately, P./Williams, J./Breda, J.
(2019). Prevalence of severe obesity among primary school children in 21 european
countries. Obesity facts 12 (2), 244–258. https://doi.org/10.1159/000500436.
Stadt Wien (2011). Bezirksgrenzen Wien:
Bezirksgrenzen, Wien Politische Landesgrenze und Bezirksgrenzen von Wien 2011. Available
online at https://www.data.gv.at/katalog/dataset/86c29af5-c52c-423d-8764-82c1bb037936.
Stadt Wien (2012). Landesgrenze Wien: Politische
Landesgrenze von Wien 2012. Available online at https://www.spatialanalysisonline.com/HTML/index.html?classification_and_clustering.htm.
Stringer, C. (2016). The origin and evolution of
Homo sapiens. Philosophical transactions of the Royal Society of London. Series B,
Biological sciences 371 (1698). https://doi.org/10.1098/rstb.2015.0237.
Swinburn, B./Egger, G./Raza, F. (1999). Dissecting
obesogenic environments: the development and application of a framework for identifying
and prioritizing environmental interventions for obesity. Preventive medicine 29 (6 Pt
1), 563–570. https://doi.org/10.1006/pmed.1999.0585.
Tanner, J. M./Eveleth, P. B. (1976). Urbanization
and growth. In: G.B. Harrison/J. B. Gibson (Eds.). Man in Urban Environments. Oxford,
Clarendon OPress, 144–166.
Thaker, V. V. (2017). Genetic and epigenetic
causes of obesity. Adolescent Medicine 28 (2), 379–405.
Timmermans, J./Dijkstra, C./Kamphuis, C./Huitink,
M./Zee, E. van der/Poelman, M. (2018). ’Obesogenic’ school food environments? An urban
case study in The Netherlands. International journal of environmental research and
public health 15 (4). https://doi.org/10.3390/ijerph15040619.
Ulijaszek, S. J. (2007). Obesity: a disorder of
convenience. Obesity Reviews 8 Suppl 1, 183–187. https://doi.org/10.1111/j.1467-789X.2007.00339.x.
Ulijaszek, S. J./Lofink, H. (2006). Obesity in
biocultural perspective // Obesity in Biocultural Perspective. Annual Review of
Anthropology 35 (1), 337–360. https://doi.org/10.1146/annurev.anthro.35.081705.123301.
United Nations (Ed.) (2015). World Urbanization
Prospects: The 2014 Revision. Department of Economic and Social Affairs, Population
Division. ST/ESA/SER.A/366. Available online at https://www.un.org/en/development/desa/publications/2014-revision-world-urbanization-prospects.html
(accessed 4/6/2021).
Vlahov, D./Freudenberg, N./Proietti, F./Ompad,
D./Quinn, A./Nandi, V./Galea, S. (2007). Urban as a determinant of health. Journal of
Urban Health 84 (3 Suppl), i16-26. https://doi.org/10.1007/s11524-007-9169-3.
Wang, Y. C./McPherson, K./Marsh, T./Gortmaker, S.
L./Brown, M. (2011). Health and economic burden of the projected obesity trends in the
USA and the UK. The Lancet 378 (9793), 815–825. https://doi.org/10.1016/S0140-6736(11)60814-3.
Wang, Y./Beydoun, M. A. (2007). The obesity
epidemic in the United States‐gender, age,
socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and
meta-regression analysis. Epidemiologic reviews 29, 6–28. https://doi.org/10.1093/epirev/mxm007.
Wang, Y./Lobstein, T. (2006). Worldwide trends in
childhood overweight and obesity. International Journal of Pediatric Obesity 1 (1),
11–25. https://doi.org/10.1080/17477160600586747.
WHO (2000). Obesity: preventing and managing the
global epidemic. Geneva, WHO.
WHO (2010). World Health Organization Global
Database on Body mass index. Geneva, WHO.
WHO (2020). World Health Organization. Obesity and
Overweight. Geneva, WHO.
Wilkinson, T. J./Philip, G./Bradbury, J./Dunford,
R./Donoghue, D./Galiatsatos, N./Lawrence, D./Ricci, A./Smith, S. L. (2014).
Contextualizing early urbanization. Settlement cores, early states and agro-pastoral
strategies in the fertile crescent during the fourth and third millennia BC. Journal of
World Prehistory 27 (1), 43–109. https://doi.org/10.1007/s10963-014-9072-2.
Withrow, D./Alter, D. A. (2011). The economic
burden of obesity worldwide: a systematic review of the direct costs of obesity. Obesity
Reviews 12 (2), 131–141. https://doi.org/10.1111/j.1467-789X.2009.00712.x.
Wolin, K. Y./Colangelo, L. A./Chiu, B.
C.-H./Gapstur, S. M. (2009). Obesity and immigration among Latina women. Journal of
immigrant and minority health 11 (5), 428–431. https://doi.org/10.1007/s10903-007-9115-1.
Zehetmayer, M. (2013). Health, market integration,
and the urban height penalty in the US, 1847‐1894.
Cliometrica 7 (2), 161–187. https://doi.org/10.1007/s11698-012-0085-8.
Zong, X./Li, H./Zhang, Y.-Q./Wu, H. (2017).
Narrowing urban-suburban rural disparities in physical growth among children in China:
findings from the 5th national survey in 2015. Annals of human biology 44 (7), 636–641.
https://doi.org/10.1080/03014460.2017.1358394.